Read the latest Vetora news and find handy animal resources here.
Our Vetora team is committed to delivering exceptional, client‑focused care across all eight of our Waikato clinics. If you have any concerns this summer — big or small — we’re always happy to help.
Book an appointment or contact your nearest clinic anytime.
Pets

Summer in New Zealand is a wonderful time to explore the outdoors with your pets—but our hot, humid weather also brings a serious risk: heatstroke. Heatstroke in dogs and cats is a life‑threatening emergency where body temperature rises dangerously above 40°C and organs begin to fail. Quick action can save a life.
This guide explains the early warning signs, severe symptoms, first aid steps, and simple prevention tips to help keep your pets safe through the warmer months.
Recognising heatstroke early can prevent a medical emergency. Watch for:
If you notice any of these, act fast—move your pet to a cooler environment and contact your vet.
Heatstroke can escalate rapidly. If your pet shows any of the following symptoms, this is an emergency:
Immediate veterinary treatment within 90 minutes leads to the best outcomes.
While organising emergency veterinary help, take these steps:
Get your pet into shade or an air‑conditioned space as quickly as possible.
Use cool, damp cloths on the paws, groin, and belly. A fan can also help.
Avoid ice‑cold water or wrapping in large wet towels, as this can trap heat.
Provide small sips of cool water—but never force drinking.
Call your local veterinary clinic or emergency vet while cooling your pet and continue cooling during transport.
Heatstroke is preventable with a few simple precautions:
In a New Zealand summer, the inside of a parked car can reach over 50°C in under 15 minutes, even in the shade and with windows cracked. This is deadly for pets and can cause irreversible heatstroke very quickly.
By recognising the early signs of heatstroke and taking simple preventative steps, you can help ensure your pets enjoy a safe, happy Kiwi summer. If you ever suspect heatstroke, always call your vet immediately—rapid action saves lives.
Pets
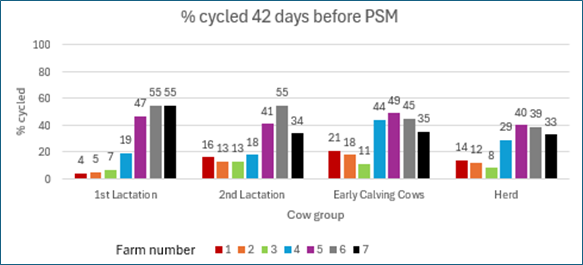
Wearable technology is transforming herd management, but the real power lies in how you use the data. At Vetora, we help farmers turn insights into action—starting with pre-mating heat detection up to 42 days before mating begins.
Recent data from seven Waikato farms shows a wide variation in pre-mating cycling rates. For example, Farm 1’s first-lactation cows were only 4% cycled, compared to 16% for second-lactation cows. Meanwhile, Farm 7 had 55% of first-lactation cows cycled versus 34% for second-lactation cows. Why such differences? Every farm has unique factors, and the solutions need to be tailored.
By analysing your wearable data, we can identify these gaps early and create a plan to improve reproductive performance. Better data means better decisions—and better results for your farm.
Ready to make your data work harder? Contact Vetora today and let’s boost your herd’s performance.
Farming

As we head into summer, it’s time to plan ahead for your herd’s health and productivity. Here are key steps for cows, heifers, and calves to keep your farm running smoothly.
Look after yourselves in the sun, and hopefully, you get a well-deserved break off-farm. Wishing you a safe and happy Christmas and New Year!
Farming

Liver Abscess in Heifers: What Waikato Farmers Need to Know
In September, a sick R2 heifer was reported in Otorohanga after rapid deterioration. Despite initial treatment with Engemycin and B12/Selenium, her condition worsened to the point she couldn’t walk back to the yards.

A post-mortem revealed severe emaciation and multiple encapsulated liver abscesses, some up to 6cm in diameter. One abscess had ruptured near the liver’s main blood supply, causing localised peritonitis and a toxic reaction that led to her decline.
Liver abscesses can occur in any age or breed of cattle but are most common in feedlot or grain-fed animals. The primary cause is rumen acidosis, often triggered by a sudden diet change from roughage to high-grain feed. Other causes include:
The bacteria responsible, Fusobacterium necrophorum, proliferates when the rumen lining becomes inflamed, allowing bacteria to enter the bloodstream and seed in the liver.
These heifers had been fed meal during winter, making rumen acidosis the likely cause. In most cases, liver abscesses remain small and only reduce growth rates. However, when an abscess ruptures near major blood vessels, it can cause rapid deterioration and death.
This case highlights the importance of careful feed management to prevent liver abscesses and protect herd health.
Farming

Horn Management in Waikato Dairy Farming: Why It Matters
Horns are permanent pointed growths made of a bony core covered by a keratin sheath, similar to a fingernail. They grow from a coronary ring on the head of cattle and continue throughout the animal’s life. While horns serve natural purposes - such as social status, communication, defence, and even thermoregulation - in modern intensive farming systems, they create significant welfare and safety challenges.
In close-contact environments like milking yards or feed pads, horns can cause injuries to other cows, bruising during transport, and even harm to humans. Common issues include:

One of the most common procedures in spring is disbudding dairy replacement calves at 3 - 6 weeks old. Under Animal Welfare Regulations, this must be done with local anaesthetic before using a hot iron to cauterise the horn growth ring. Older animals with large or deformed horns may require dehorning, which is more complex and often involves sedation and local anaesthetic.
Horn growth is controlled by genetics. A dominant gene produces polled (hornless) cattle, while a double recessive gene results in horned animals. Many beef breeds like Angus and Hereford have been selected for polled genetics. Using these bulls over dairy cows can significantly reduce the need for disbudding.
The challenge: Invest in polled dairy genetics. Within a few years, your herd could be entirely polled, improving welfare and reducing risk for both animals and people.
Farming

Parvovirus is a highly infectious and often deadly virus that mainly affects puppies and unvaccinated dogs. It is resistant to normal disinfection and can survive in the environment for months to years, depending on humidity and temperature.
Some dogs may be subclinically infected, meaning they carry the virus without appearing sick—making it easy to spread. It only takes a tiny amount of virus to infect a new host.
How It Spreads:
The virus is shed in the faeces of infected dogs, and symptoms usually appear 3–7 days after infection.
Parvovirus attacks:
Without treatment, the mortality rate for puppies is around 91%.
If you notice any of these signs, contact your vet immediately—early treatment greatly improves survival chances.
Vaccination is the safest way to protect your pet. Adult dogs rarely get Parvo thanks to widespread vaccination, but yearly boosters are often recommended during annual check-ups.
✅ Check your pet’s vaccination status for Parvovirus, Kennel Cough, and Canine Distemper.
✅ If you’re unsure, call your local vet clinic—we’re happy to help.
✅ Share this post to protect other pets in your community.
📞 Talk to us today about protecting your pet from Parvo!
Pets

Wishing you a successful end to mating and a healthy, productive season ahead.
Farming

Amino acid nutrition in dairy cows is a critical component of optimising milk production, reproduction, and metabolic health. In New Zealand, the challenge lies in balancing amino acids within high-protein, grass-based systems, which differ significantly from the Total Mixed Ration (TMR) systems used in other parts of the world.
Proteins are made up of amino acids (AAs), and 10 of these are essential—meaning they cannot be synthesised by the cow and must be obtained through the diet. Among these, methionine (Met) and lysine (Lys) are typically the first- and second-limiting amino acids in dairy cow diets. When deficient, they can restrict protein synthesis, even when dietary crude protein (CP) is sufficient.
Imbalanced amino acid profiles can:
To provide methionine and lysine in New Zealand dairy systems, farmers can use rumen-protected (bypass) amino acid products. These are formulated to withstand ruminal digestion and be absorbed in the intestine.
When selecting products, it’s important to consider:
These factors help determine the appropriate supplementation levels.
Supplementing amino acids is not just about quantity—it’s also about the correct ratio. A lysine-to-methionine ratio of approximately 3:1 in the metabolizable protein (MP) is often considered ideal for milk protein synthesis.
In practical terms, some trials have used:
It is advisable to supply methionine and lysine during critical physiological periods, such as:
Farming

Earlier this year, our veterinary team was called out to a Waikato dairy farm after a group of cows broke into a stack of mouldy maize. A few days later, several cows began showing signs of illness, prompting an urgent on-farm visit.
One cow was found down in the paddock, displaying concerning symptoms:
We immediately administered supportive care, including:
Meanwhile, other affected cows remained standing but presented with:
Given the recent maize consumption, rumen acidosis was a primary suspect. However, we also considered:
To confirm the diagnosis, we collected faecal samples for laboratory testing.
Both rumen acidosis and Salmonella can cause foul-smelling diarrhoea. However, there are key differences:
Regardless of the cause, fluid therapy with electrolytes is essential to replace losses and support recovery.
Lab cultures confirmed the presence of Salmonella. Interestingly, the strain identified in this outbreak was Salmonella Give, while the previous outbreak had been caused by Salmonella Typhimurium. This indicated two separate outbreaks, not a continuation of the same infection.
Given the recurrence, we recommended vaccinating the herd. Although the vaccine does not currently include the Salmonella Give strain, which is relatively new, there may be some cross-protection. Vaccination during an outbreak is still considered beneficial to limit spread and protect unaffected animals.
To reduce the risk of Salmonella outbreaks in your herd:
This case highlights the importance of early intervention, accurate diagnosis, and proactive prevention in managing herd health. If you suspect a Salmonella outbreak or have concerns about feed safety, contact our veterinary team immediately.
Farming

Has your dog injured their knee joint, just like Damian McKenzie? In dogs, this common injury is a tear or rupture of the cranial cruciate ligament (CCL) — the veterinary equivalent of the human ACL.
The cranial cruciate ligament is one of two key ligaments in a dog’s knee (stifle) joint. It stabilises the joint and prevents internal rotation. Damage to the CCL is one of the most common causes of hind leg lameness in dogs across all breeds and sizes — not just active or athletic dogs.
If your dog has torn their CCL, surgical repair is usually required. Cage rest may help very small dogs, but it’s rarely effective for medium to large breeds.
At Vetora Hamilton, we offer two trusted surgical options to stabilise your dog’s knee and restore mobility:
This extra-articular procedure uses a suture to mimic the function of the CCL and stabilise the joint.
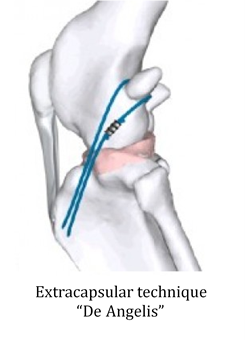
✅ Best suited for small to medium-sized dogs
💰 Cost: $1,800 – $2,200
Recommended by most orthopaedic specialists, TPLO involves reshaping the tibia to change joint loading and allow normal weight-bearing.
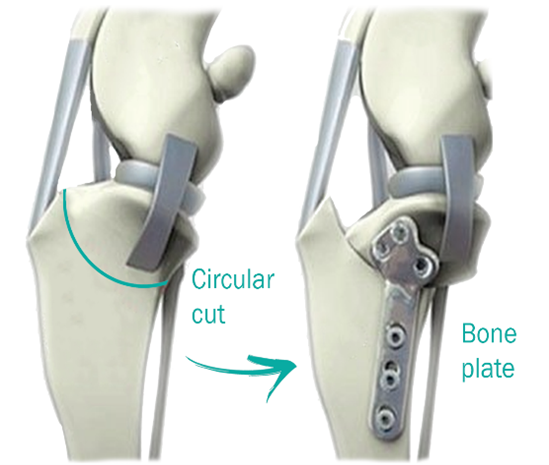
✅ Ideal for active or larger dogs
💰 Cost: Approx $4,800
These advanced cruciate surgeries are offered exclusively at our Hamilton clinic, serving pet owners across the Waikato region — including Te Awamutu, Cambridge, Morrinsville, Otorohanga, Putaruru and surrounding communities.
📍 Book your dog’s cruciate surgery at Vetora Hamilton today
📞 Call us or book online to get your pet back on their feet for summer!
Pets

Lameness is a year-round challenge, but late spring can be particularly tough for Waikato and Taupō dairy farmers. With mating season approaching, lame cows can cause:
Before the rush of mating, take time to reduce lameness issues and keep your herd moving.
Early identification of lame cows is key to faster recovery and better animal welfare. Hoof problems often start small and worsen over time. If you catch and treat them early:
Tip: Train farm staff to check for lameness every time cows walk to and from the shed. Mark and draft affected cows promptly for examination.
When treating a lame cow, the most important step is to lift the foot and inspect it. Skipping this step and going straight to antibiotics can:
Most lame cows do not need antibiotics. Common causes in NZ include:
Only digital dermatitis and foot rot consistently require antibiotics. The rest can often be treated with hoof trimming, pain relief, and time.
Learning to diagnose and trim hooves is a valuable skill. Our Taupō veterinary team can:
Contact your local Waikato or Taupō vet clinic for advice, treatment, or to book a training session.
📞 Call us today – let’s keep your cows moo-ving this season!
Farming

When a farmer in Tokoroa, Waikato called about a five-week-old Friesian cross Jersey calf with a “blimp-sized” abdomen, our team knew immediate action was needed. The calf had:
These signs indicated significant pain and possible gastrointestinal complications.
We passed a stomach tube to rule out oesophageal impaction and relieve any free gas. The tube entered the rumen easily, eliminating an oesophageal blockage. Only a small amount of gas was released, ruling out free gas bloat. Green liquid in the tube also ruled out ruminal milk drinking bloat.
We opted for conservative treatment:
The calf improved overnight, and the bloating reduced significantly. The most likely cause was:
If you suspect bloat in calves, call your local Waikato vet clinic immediately. Early intervention saves lives.
📞 Contact us today for advice or emergency support.
Farming

When it comes to drenching calves for worms and managing coccidiosis, timing is everything. But in New Zealand—especially here in the Waikato—there’s still a lot we don’t know about the best time to start.
That’s why this spring 2025, our veterinary team is launching a regional study to help answer some of the most common questions we hear from local farmers:
We’re inviting farmers across the Waikato to participate in a collaborative study aimed at improving calf health and parasite management. As part of our Lepto vaccination visits, we’ll:
You’ll receive a personalised report with your farm’s results, and we’ll compile anonymised data across all participating farms to identify trends and best practices.
By participating, you’ll help us answer key questions and improve parasite control strategies for the entire region. The benefits include:
If you’d like to be part of this important study—or if you just want to chat about your calf drenching programme—we’re here to help.
📞 Contact your local clinic today to get involved or learn more.
Together, we can build a healthier future for our calves and our communities.
Lifestyle
Farming

With a wide range of drenches available on the market, choosing the right one for your calves isn’t just a matter of preference—it’s a critical decision that can significantly impact their health, growth, and long-term productivity.
Drenching plays a vital role in calf rearing. Worm infestations can reduce growth rates by up to 30%, primarily due to appetite loss and poor nutrient absorption. Common symptoms include:
Unchecked worm burdens can escalate into serious conditions such as parasitic gastroenteritis, bronchitis, or pneumonia—especially when lungworm is involved.
From weaning through to around 15 months of age, calves are particularly susceptible to parasites. Their immune systems are still developing, leaving them less equipped to fight off infections. This makes early and effective parasite control essential.
When it comes to young stock, quality should never be compromised. High-quality drenches are backed by:
In contrast, cheaper drenches may result in:
Saving a few dollars upfront can lead to long-term losses in productivity and animal health.
Purchasing your drench through your veterinarian ensures you receive expert, tailored guidance. Vets consider:
They can also help you:
Veterinary support is not just about choosing a product—it’s about building a sustainable parasite control strategy. This is crucial for:
Lifestyle
Farming
Farming

Synchronising heifers isn’t for everyone – it’s a lot of extra work at a busy time of year. But the economics of getting extra replacement heifer calves from your highest BW animals and increased days in milk do make it worthwhile, if you decide to do it.
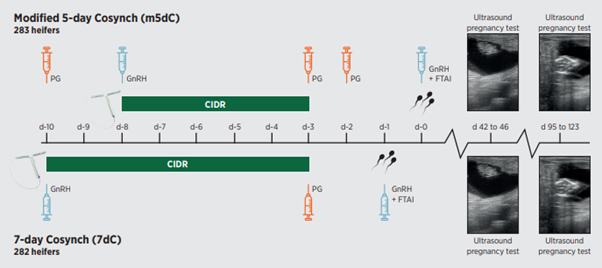
There are several synchronisation programmes available for dairy farmers in the Waikato region. While many have been used for years, the Modified 5-Day Cosynch Programme shows significant improvements over the standard heifer CIDR synchrony programme, the 7-day Cosynch.
Looking at the table and graph below, there is an increase in conception rate to AI from 45.5% with the standard programme to 62% with the modified 5-day Cosynch.
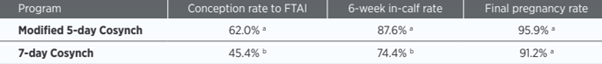
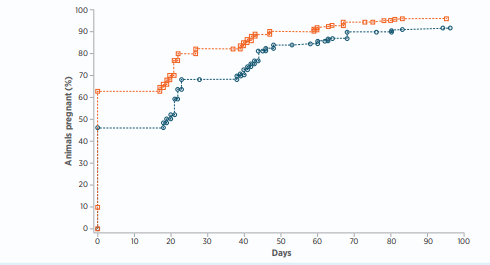
The downside (there is almost always a downside) is 5 yardings during the 10 days of the programme, compared to 3 yardings for the old programme. There is also an increase in cost for the extra 2 PG injections. The table below shows the timing of both programmes.
There are a couple of other options for synchronising heifers that don’t involve CIDRs. They are:
If you're considering heifer synchronisation in Waikato, King Country, or surrounding areas, contact your local Vetora clinic. Our experienced veterinary team can help you choose the most effective and cost-efficient programme for your herd.
Farming

A two-year-old Friesian cross steer in the Waikato region recently presented with lameness in his right hind leg. The steer was part of a mob of twelve similar age steers that had arrived on the property as yearlings. Upon examination, the steer showed inflamed, thickened skin between the heel bulbs. There was no interdigital footrot between the claws - leading to a diagnosis of Bovine Digital Dermatitis (BDD).

BDD is a contagious bacterial infection caused by Treponema species. It’s the most important infectious cause of lameness in cattle worldwide, first identified in Italy in 1974 and diagnosed in New Zealand dairy herds in 2004. Since then, it has spread across all major dairy regions, including Waikato and King Country. One study in Taranaki found 2/3 of 224 herds examined had at least one cow with BDD.
BDD typically affects the back feet and causes damage to the skin between the heel bulbs or along the coronary band.
Wet, muddy conditions—common in the Waikato region—combined with faecal contamination on races, yards, and feedpads, significantly increase the risk of infection. Infected cattle can spread BDD quickly, making quarantine and biosecurity essential and checking stock before arriving on-farm are useful preventative measure.
In the case above, the steer was treated with:
Early diagnosis and treatment are crucial to prevent herd-wide outbreaks.
To reduce the risk of BDD on your farm:
If you're farming in Ōtorohanga, Te Awamutu, Putaruru, Tokoroa, Cambridge, Hamilton, or anywhere in Waikato or King Country, contact your local Vetora clinic. Our experienced vets can help you:
Farming

Weaning is a pivotal stage in calf rearing that directly influences lifetime performance. For farmers across Waikato and King Country, successful weaning requires more than just removing milk—it demands careful attention to nutrition, rumen development, parasite control, and stress management.
Weaning should be based on liveweight and rumen development, not age alone.
High-quality calf meal or pellets rich in starch and protein stimulate rumen papillae growth, improving nutrient absorption.
Ensure calves are confidently eating pasture and meal before weaning.
Look for:
Water is vital for rumen function and overall calf health.
Ensure constant access to clean, fresh water.
Calves are highly susceptible to worm burdens after weaning.
Young calves need leafy, high-energy pasture—not mature or fibrous grass.
This supports continued growth and development.
Handle calves calmly and keep groups stable.
Avoid weaning during poor weather or feed shortages.
Successful weaning is about more than just removing milk.
Balancing nutrition, parasite control, and stress management—along with proper weight and rumen readiness—ensures calves transition smoothly and continue on a path to strong lifetime productivity.
Well-grown heifers make well-grown cows.
Whether you're farming in Te Awamutu, Ōtorohanga, Putaruru, Tokoroa, Cambridge, Hamilton, or surrounding areas, your local Vetora clinic is here to support your calf rearing success. Contact us for tailored advice, drenching plans, and growth monitoring tools.
Farming
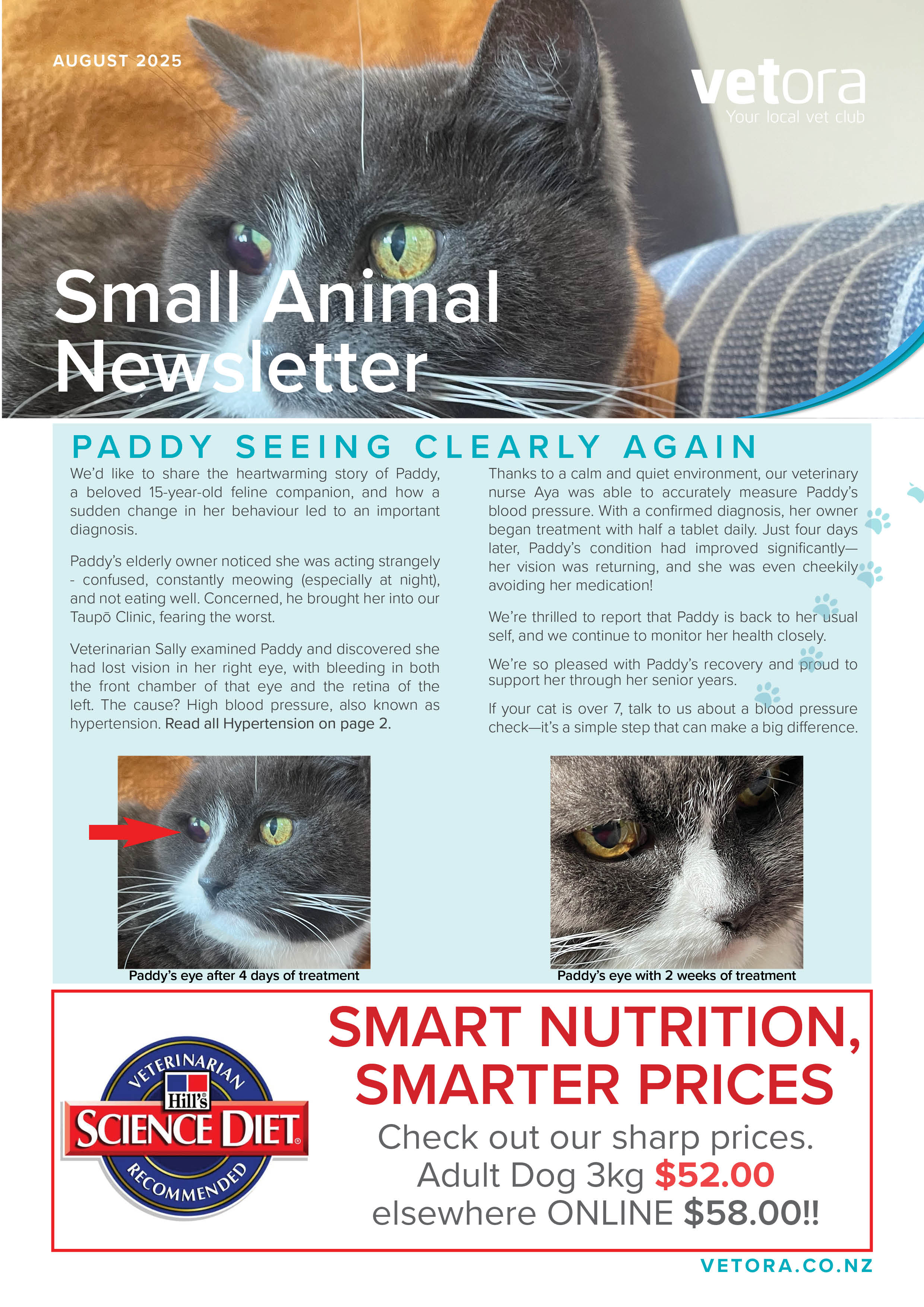
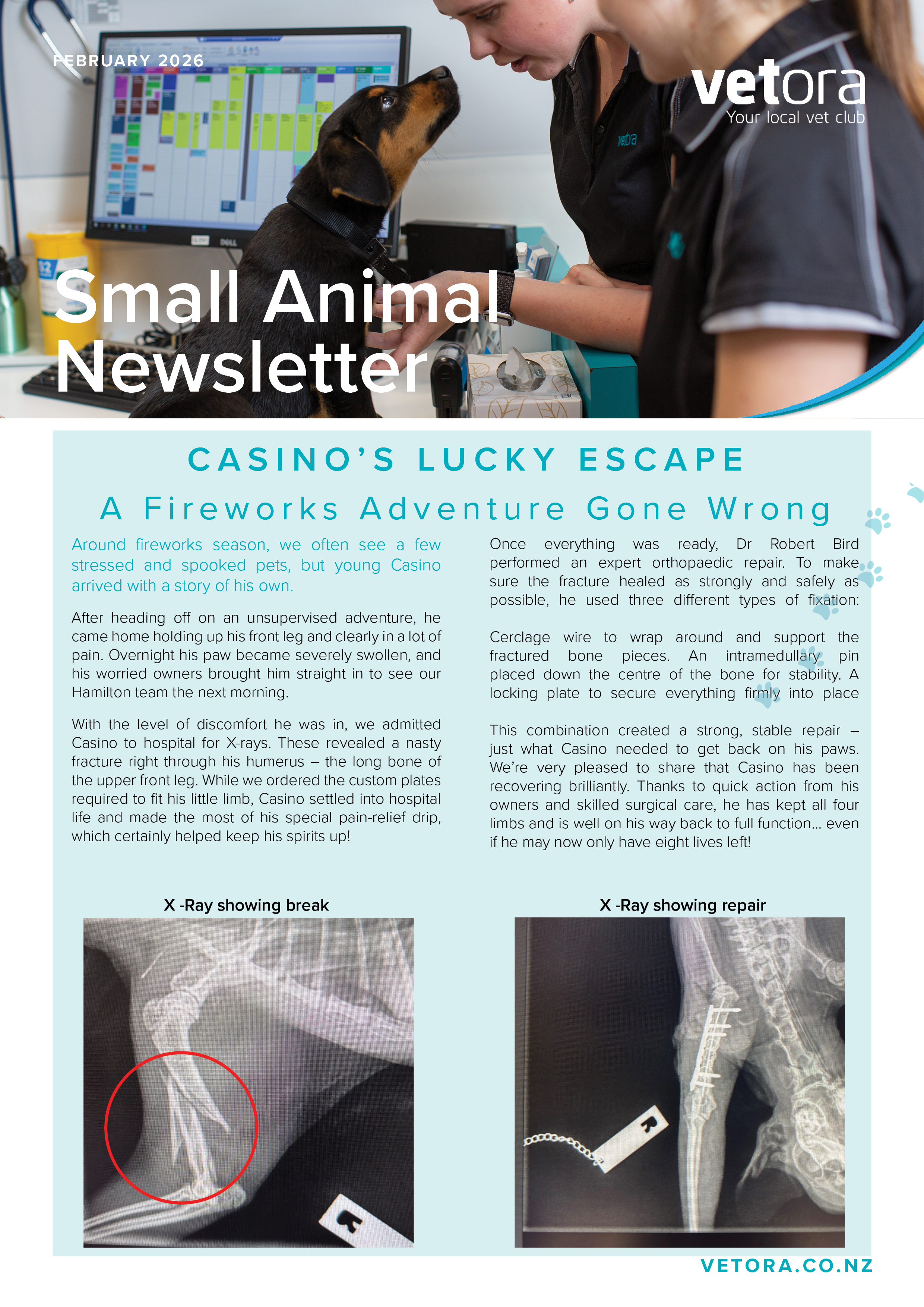
We’re excited to share the latest edition of our quarterly Small Animal Newsletter, packed with updates, insights, and a few treats for our pet-loving community!
Here’s what you’ll find inside this issue:
Take advantage of our current promotions on selected products and services – perfect for keeping your furry friends happy and healthy as we head into the new season.
This quarter’s spotlight dives into a fascinating case from one of our clinics, showcasing the teamwork, diagnostics, and care that go into helping our patients thrive.
Get to know one of our amazing team members! We love introducing the people behind the scenes who make our clinics such a special place for pets and their owners.
Thank you for being part of our community – we’re proud to serve the pets and people of the Waikato with care, compassion, and clinical excellence.
Pets

We’re pleased to share the latest edition of our monthly Focus on Dairy newsletter, created especially for our farming community across the Waikato.
This month’s issue is packed with valuable insights and practical updates, including:
A real-world example from one of our production animal vets, highlighting diagnostic challenges and treatment outcomes on-farm.
Take advantage of current offers on selected products and services to support herd health and farm efficiency.
Stay informed with the latest developments in dairying – from seasonal herd management tips to emerging technologies and best practices.
Whether you're a long-time client or new to our clinics, Focus on Dairy is designed to keep you connected, informed, and supported in your day-to-day operations.
Thanks for being part of our farming community – we’re proud to support the people and animals that power the Waikato.


Farming

One Thursday afternoon in September, I was called out to see a cow in distress. She was down in the yard, groaning, and severely bloated—so much so that I feared she might die from bloat right in front of me.
My first priority was to relieve the gas pressure in her rumen. After confirming it was free gas with a needle (a continuous hiss confirmed this), I administered a local anaesthetic and inserted a red plastic trocar. The gas released quickly, but the cow still looked unwell.
I began a full clinical exam. She was due to calve in about five days, and my checks confirmed the calf was still alive. Suspecting a possible blockage, I passed a stomach tube, which went down easily—ruling out an obstruction. However, the cow reacted poorly, groaning and rolling, which added to the puzzle.
As I stood back and reassessed, her symptoms—bloat, weakness, and depression—pointed to hypocalcaemia (milk fever). It was unusual to see such extreme bloat with milk fever, especially in a cow that hadn’t calved yet. Still, I decided to administer intravenous calcium.
The response was almost immediate. Her condition improved visibly during the infusion, and she was up and walking not long after I left. A few days later, she calved a healthy calf.
Thanks to Cow Manager wearables on this farm, we could review her activity data. The day before the incident, she hadn’t eaten or moved much—clear signs of early illness. This lack of intake during the critical transition period likely triggered the milk fever, even before calving.
This case was one of the most unusual presentations of milk fever I’ve seen—but with quick action and the right diagnosis, it had a successful outcome.
Farming

Calves are creative creatures, and anyone who has done calvings knows they can find any number of interesting positions to cause a problem to the cow when they enter the world. Occasionally though, the issue lies not with the calf itself, but actually with the uterus.
Uterine torsions occur when the body of the uterus twists around at the level of the cervix and can range from 90 to 360 degrees. The twist both narrows the birth canal, and prevents the cervix from dilating properly. Cows with a uterine twist are basically stuck in stage 1 of labour (cervical dilation) and will not be able to progress to stage 2 (birth of the calf) until the twist is corrected.
In a partial or “open” twist, the cervix will be partially dilated, and you will be able to feel the calf. However the calf will often be either on its side or upside down. The twist may be difficult to distinguish from a poorly dilated cervix, but you may find that your arm drops away to the left or right as you enter the cow. These cows can often be untwisted standing, your vet may untwist them by hand, or using a Gyn stick or torsion rod.
In a complete or “closed” twist, the uterus has twisted down to a complete closure, which can easily be confused with a closed cervix. Cows with a twist of this severity either need to be cast and rolled (essentially rolling the cow around the calf) or have a c section. The key to a successful roll is having plenty of hands to help.
Once untwisted, the next problem to tackle is a poorly dilated cervix. Think of the calf as a loaf of bread, the uterus as a bread bag, and the cervix as the bread tag. Even if you untwist the bread bag, you can’t get to the bread without removing the tag! In a live or freshly dead calf, there is often a good chance the cervix will dilate. With a rotten calf, the chance of dilation is very low and prognosis is poor.
Always consider the possibility of a twisted uterus if a cow is not progressing as quickly as you expect. These cows will not tend to visibly strain or push because the calf is not able to enter the birth canal. Early detection and correction will always give the best chance of a good outcome.
Farming

A bone sequestrum is a portion of dead bone which generally occurs due to direct trauma to bone. Bone sequestrums are not very common and can be seen 2-3 weeks after injury.
How they do they occur?
Direct trauma damages cortical bone (outer layer of bone) which causes bone death due to loss of blood supply and bacterial infection.
What does it look like?



The animal may show mild to moderate lameness. They are often non-healing wounds which can respond to antibiotics but recur once the antibiotic course ends. We often see pus coming from a small drain hole on the leg wound.
How is it diagnosed?
History of trauma, draining tracts and non-healing wounds. We can also ultrasound or radiograph the leg to identify damaged bone.
- Radiograph: Abnormal bone circled.
- Ultrasound: Normal, smooth bone (white curve) is displayed on the left. Sequestrum is displayed on the right where the bone is interrupted (red arrow).
How do we treat this?
Surgery is required to remove the damaged portion of bone. Without surgery, the dead bone acts as foreign material causing a persistent source of irritation and infection
Farming

Farmers are familiar with the common presentation of abscesses as the cause of rapidly growing masses on their cattle, but not all are as they seem. It is important for abscesses to be diagnosed and treated properly. This may include a needle aspirate to confirm pus is present, local anaesthetic to provide pain relief, thorough cleaning of the skin before incision, stand back for a fountain of pus and a good flush, finishing up with the old faithful- blue spray. Antibiotics are not usually required.
This case involved a call for a lump with quite a different outcome. This heifer had a small lump (golf ball sized) as an R1, that was presumed to be a small abscess and left to heal. The lump had stayed the same size for a while, and then in the last 3 weeks or so (as an R2 heifer) had rapidly grown.
The Friesian heifer had a mass on her shoulder, approximately the size of a soccer ball on presentation. As she came through the yards the skin split to reveal bleeding, shiny black tissue. The appearance indicated that the mass was in fact a melanocytoma- a tumour of pigment producing cells. These tumours can grow to impressive sizes and are unable to be transported to the works if the skin is split, which they are prone to doing.
The heifer was prepared for surgery- clipped, cleaned and local anaesthetic ring block applied. The tumour was cut off, sewn up, then pain relief and antibiotics were given to the heifer. At that point she looked brand new but be warned, this surgery can create a blood bath! Sutures were removed after 14 days, she recovered well and was still in calf.
Melanocytomas are an uncommon cancer of cattle (about 5% of all cancers in bovines) and occur usually in young animals. Dark coloured breeds e.g. Angus, Friesian etc are especially prone. Most melanocytomas in cattle are benign, and surgical excision is curative. Approximately 20% of cases may feature spread to lungs or lymph nodes. These tumours are prone to bursting open which then means the animal is unsuitable for transportation to the works. They are often very vascular (can contain abnormal blood vessels) which in rare cases can result in huge blood loss. Surgery is the only curative option, with wide surgical margins the prognosis is good, recurrence is possible but uncommon.
Farming

The transition period is defined as the timeframe from 4 weeks before calving until 4 weeks after calving and is characterised by an increased risk of disease. The changes in metabolic status have a long-term effect on the health, fertility and productivity of dairy cows. Most metabolic conditions, such as milk fever, ketosis, primarily affect cows during this period as do disorders such as RFMs, metritis, displaced abomasum and lameness.
Feed intake and nutrient density of the diet determine the nutrients available to the cow and developing foetus, so cows need enough energy for them and the foetus. During the last month of gestation cows (550kg bodyweight) should be provided with at least 8 to 10 kg DM in feed, providing at least 10 MJ/kg DM, to allow for foetal growth without depletion of the cow’s body stores. Over feeding cows prior to calving can predispose cows to milk fever, udder oedema and mastitis.
It is recommended that cows are dried off in the BCS they are required to calve. A BCS 5 for cows, 5.5 for heifers are considered optimum to achieve the best results in terms of subsequent production and reproduction. Cows at or above target BCS should be fed 90 percent of their daily energy requirements for two to three weeks before calving. Cows that are below target BCS should be fed 100 percent of their daily energy requirements.
The management of the transition diet is important to reduce the risk of milk fever. Pastures high in potassium and sodium should be limited due to their detrimental effect on the DCAD, so avoid access to effluent paddocks. Adequate magnesium and phosphorus also need to be provided in the late dry period.
There are a range of ways to supplement with magnesium – magnesium oxide can be mixed in feed or dusted on pastures; magnesium sulphate and magnesium sulphate can be added to the drinking water. Cows need to adjust to treated water - so slowly introduce it, as high levels make the water unpalatable. Also, magnesium intra-ruminal bullets can be used - they release magnesium over 9-12 weeks.
Dairy cows have a level of immunosuppression due to the period immediately before, during and after calving. This means they are more susceptible to disease, and this can be made worse by inadequate trace element nutrition. Aim for optimal levels of selenium, copper, and zinc.
The goals of nutritional and environmental management during the transition period are to maximise the appetite of the cow just before and after calving, minimise body fat mobilisation around calving, maintain calcium at and after calving, and to maintain or enhance the animal’s immune function.
Farming

As the colder months settle in, it’s not just us feeling the chill — our pets do too!
You might notice your furry friends slowing down a little more than usual.
Stiffness, moving slower
Reluctance to move, climb stairs
Repeatedly licking at joints
Just seeming a bit “off”
These can all be signs that the cooler weather is affecting their joints.
We’re here to help. There are lots of options to help support joint health in our pets and we recommend discussing with you vet about which options are best for you and your pet.
If you’re noticing any changes in your pet,or just want to chat about how to keep them comfy this winter, give your local Vetora clinic a call. We’re always happy to help!
Pets

Heifers are home from grazing - is there liver fluke lurking?
From testing over the years we have found Liver fluke infection in grazing heifers, particularly from the King Country and areas where cattle graze on wet marshy pastures and margins of streams. The problem is that once infected, the adult fluke will live for years in your cows.
Often the first indication will be the presence of liver fluke on the killing sheet from cull cows. These are usually old flukes that have been living in the liver since they were grazing heifers.
Low levels of liver fluke cause decreased fertility, increased susceptibility to other diseases and parasites as well as decreased weight gain in growing cattle, and decreased milk production.
If you would like to know if you have an active infection in your heifers, a blood test from a group of animals will provide the answer.
Controlling fluke requires a flukacide and these drugs have a significant milk withhold so treatment needs to be carried out well before calving.
Drenching with Flukecare + Se is the most effective treatment, killing adult and immature fluke, BZ sensitive intestinal worms and four weeks of Selenium supplementation. It has a milk withholding of 35 days and meat and bobby calves of 28 days.
Alternatively, Ivomec Plus injection is effective in the control of adult fluke as well as mectin sensitive intestinal parasites and lungworm, as well as aiding in the control of lice. It has a milk withholding of 14 days and meat and bobby calves of 28 days.
https://nz.virbac.com/products/parasiticides-drenches/flukecare-plus-se#image
Farming

Abscesses in cows are localised, pus-filled infections that can develop due to injury or infection, or bacteria entering the body through open wounds or compromised skin. An abscess is a defence mechanism that helps prevent the spread of infection to other parts of the body. Abscesses have a wall, or capsule, that is formed by adjacent healthy cells in an attempt to keep the pus from infecting neighbouring structures. However, this capsule will also prevent immune cells and antibiotics from reaching the bacteria in the abscess.

Abscesses usually appear as firm, swollen lumps, often found around the neck, shoulder, flank or the back of the legs, but can occur on almost any part of the body. They may start small but can grow rapidly. It is not uncommon to see an abscess the size of a football, containing upwards of five litres of pus.
Many cows with abscesses appear otherwise healthy, but, if left untreated, an abscess is likely to cause discomfort, disrupt milk production, and even lead to systemic infection.

The most important aspect of treatment involves lancing and draining the abscess, ideally by a veterinarian. An X-shaped hole is recommended to prevent the wound sealing shut too early, which could allow the abscess to fill up again. Where possible, the hole should be located to enable it to drain freely via gravity, and it should be big enough to insert a finger into the abscess to allow exploration for foreign bodies (sticks, bits of wire, pieces of bone, etc) or pieces of firm pus or necrotic tissue that can block the hole and impede drainage.
The abscess should be thoroughly flushed, ideally with dilute iodine or chlorhexidine, but if drainage of the abscess is good, tap water will be ok.
I would strongly recommend administering local anaesthetic before lancing an abscess, as it is necessary to make more than one cut through thick cow skin, sometimes also through muscle, as well as through the abscess capsule. Although the area is under pressure from the abscess, this will still be a painful procedure for the cow. An anti-inflammatory, such as Metacam or Ketomax, may also be given to provide further pain relief and help reduce inflammation and swelling at the abscess site. Antibiotics are usually not given due to the abscess capsule.
The abscess should continue to be flushed out for a further two to five days, and during this time, it is good practice to continue to explore the hole with a gloved finger to search for any objects that could contribute to the infection, or that may block the drainage hole.
Preventing abscesses can be difficult, but if there is an outbreak of abscesses with a common location, consider investigating broken gates and rails, faulty equipment, and injection hygiene and technique.
Regularly inspecting cows for signs of injury or infection is crucial, as early detection leads to easier treatment.
Farming

Warning:
A dry autumn significantly increases the risk of lethal nitrate poisoning outbreaks. Spikes in nitrate levels often occur in seasons like the one we are experiencing when seasonal conditions combine in the autumn and winter, particularly following summers and autumns that are drier than normal as rapid uptake of nitrate from the soil by plants occurs with rains following drought conditions. Nitrate levels then build up in pasture when nitrate is taken up by the plant faster than it can be converted into protein.
This can be due to deficiency in plant energy due to plant stress or low sunlight levels, especially in annual grasses and crops with a high nitrate demand. Nitrates can be absorbed quickly by plants when temperatures are low, but conversion to protein occurs very slowly during cold weather causing nitrates to accumulate. The nitrate converts to nitrite in the rumen and then binds to haemoglobin in the blood stopping it from carrying oxygen. Death can occur rapidly due to lack of oxygen to the brain.
Signs of poisoning include muscle tremors staggering and collapse but animals are often found dead. Mucus membranes and teats have a distinctive bluish chocolate colour and blood looks like dairy milk chocolate.
Surviving animals will often abort due to lack of oxygen to the foetus. To reduce the risk of poisoning cattle should not go onto newly sown pasture hungry and should have been fed something high in fibre e.g. hay or silage prior to grazing Introduce stock to high risk paddocks in the early afternoon so that plants have had the sunlight necessary to convert excess nitrate to protein. Warm, dull and overcast days will be more dangerous.
Do not leave on risky pasture overnight. Restrict grazing time to around 1 hour and control the area they have access to. Give time to adjust to the feed by gradually increasing the intake. (This gives time for the rumen microflora to adjust). Check cattle regularly for signs of poisoning. It usually takes 4-5 hours for signs to develop.
To ensure your herbage is safe can test your herbage with a nitrate test kit available from your clinic or we can test it for you. We can help by treating affected cattle with methylene blue, so if you are suspicious of nitrate poisoning or have down cows or young stock after grazing new pasture please call us immediately as time will be of the essence!
Farming

KENNEL COUGH ALERT – What every dog owner should know
CANINE INFECTIOUS TRACHEOBRONCHITIS aka “KENNEL COUGH”
What is it?
Kennel cough is a viral disease similar to the dog “flu” which can be caused by multiple different viruses and bacteria. The kennel cough vaccination your dog gets protects against some of these viruses but not all so even if they are vaccinated, they can still get the cough if another virus is going around, but often they will have milder signs.
How can my dog get it?
Kennel cough is often caught when at doggy daycare, at the groomers or around other dogs, but they still can pick it up just from walking past another dog as it is spread by small droplets from sick dogs that cough and sneeze.
Even if your dog has contracted kennel cough, they may not show any signs until 10 days after the contact. And the cough itself can last up to 2 weeks!
What does it look like?
A sudden dry hacking cough
Retching and gagging, even bringing up foam
Being “off” and a bit lethargic
Runny nose and loud snorting / sneezing
It is most important to protect young and old dogs, and this is when it can become complicated with pneumonia.
When should you come to see us?
Kennel cough can be mild and your dog may clear the virus with some TLC, however, secondary inflammation can cause a lot of discomfort and can result in your pup feeling unwell. If you think your dog may have kennel cough, please contact your clinic to assess if he or she needs to be seen.
Please DO NOT come into the clinic when you arrive, wait in your car and call us to let us know you are there.
If you want to know more, give your closest Vetora clinic a call!
Pets

We were called out to perform a postmortem on a cow that had died suddenly despite showing no symptoms prior to this. This was the second cow this had happened to, and the farmer was concerned about a serious underlying problem in the herd.
Following a thorough, systematic approach we checked the cow from nose to tail trying to find the underlying cause. We started to get concerned as everything appeared completely normal… that was, until we cut into the heart and a large spurt of pus glazed my wet weathers! This cow had a large abscess INSIDE her heart muscle!

An intramyocardial abscess. These are extremely rare and occur when bacteria make it into the blood and establish themselves inside the heart muscle. It is likely that the cow had a minor underlying infection somewhere previously, allowing the bacteria to enter the bloodstream. In this case, the abscess likely just got so large that it disrupted the electrical conduction in the heart, ultimately resulting in a heart attack. This was likely an isolated event, and we found no evidence that this presented a threat to the herd.
Farming

The answer to the question of when to dry cows off depends on your plan for winter feeding and the trade-off between production this season and next season. Having said that, the rule of thumb is :
There are a couple of tools available to help guide your decision beyond the rules of thumb:
1. Infovet dry-off planning report
2. DairyNZ milk on/dry off tool (https://www.dairynz.co.nz/tools/milk-on-dry-off/#)
Talk to your vet or local DairyNZ area manager if you would like help to use this tool.
Farming

Here is your Vetora mid-April - Spring calving e-Update
Lovely to see some rain finally after a record breaking autumn drought! Spore counts are still reasonably high and with the rain may increase, so don’t relax on the zinc just yet – those spores are tough little sods and they don’t break down as quickly as you’d like them to, even with a few cooler nights.
COWS
HEIFERS
CALVES
All the best for the last few weeks of the season.
Farming

COWS
HEIFERS
CALVES
We are looking forward to catching up with everyone soon during RVM consults!
Farming

Recently one of our farmer members noticed a tiny sore spot on his finger. A swelling quickly spread to his wrist and forearm, so he saw his doctor who referred him to hospital where he was put on intravenous antibiotics.
Despite this it quickly got worse, and tests revealed antibiotic resistant bacteria in the wound. In the end the hospital was able to change to an effective antibiotic which made a big difference. However, due to complications and delayed treatment he required surgery and was off work for weeks
Antibiotic resistance is a significant global health threat. In 2019, it was directly responsible for approximately 1.3 million deaths worldwide and contributed to nearly five million deaths. Projections indicate the number will continue to increase.
Antibiotic resistance occurs in animals too, and the impact of antibiotics from animals entering the environment also impact on humans. A concerted effort is being made by vets to reduce the use of critically important or “red light” antibiotics that are the last line of defence for some human infections.
We also aim to use antibiotics to only treat infections as antibiotics are not indicated for preventing infections.
This is particularly important when using dry cow therapy. Most cows in a herd will have a cell count below 150,000 which indicates they are not infected and don’t need antibiotics.
Teat sealants like TeatSeal don’t contain antibiotic and stay in the cow for the long run to prevent mastitis through the longest dry period and that high-risk period at calving.
Talk to your vet at your annual dairy review about how they can work with you to reduce antibiotic use on your farm.
Farming

In the midst of a particularly hot Summer you may have noticed that your working day has gotten particularly sweaty over the past few months. Now if you add a black leather jacket and pants to your attire as well as a many-fold increase in water requirement you may have some idea of how a dairy cow in a Waikato Summer feels.
Heat stress occurs when a cow’s body is unable to regulate its temperature effectively due to hot weather and/or high humidity, leading to discomfort and physiological strain. Heat stress is generally due to high air temperatures, especially those above 25°C though other factors like humidity, direct exposure to sunlight and lack of ventilation can amplify the effects. Below is the Temperature Humidity Index (THI) which you can use to assess your herd’s risk of heat stress on a given day.

Heat stress may manifest in your herd as shade seeking, gathering at water sources, panting and drop in milk yield through to collapse and death in extreme cases. It is also a common cause of early abortion which explains some of the empty cows that never cycled again after mating that we find during summer scans.
So what can you do?
In this particularly hot Summer you will never fully combat the effects of heat stress but there is plenty you can do to help. Remember that if it’s hot for you, it’s hot for them!
Farming


Does your cat or dog get very anxious when visiting the vets? Here are a few pointers that may help reduce the stress for both you and your pet.
Dogs:
Call in to the clinic when not having a checkup to have staff give a treat to increase the times your dog comes without anything negative happening to them. Some dogs may be able to be examined in the car or car park – check with your clinic if this is possible on arrival.
DAP – dog appeasing pheromone can be purchased in the clinic to spray in the car on the way to the clinic.
Calmex tablets can be bought without a prescription to help mild cases of anxiety, just ask the reception staff as it is kept in our drug dispensary.
Anxiety medications – we can script out medications to give your dog an hour or two prior to their appointment to help take the edge off their anxiety. Examples include Gabapentin, Trazadone and Lorazepam at varying doses. Ask your vet about what “Chill protocol” is best for your dog.
Cats:
Feliway spray – this can be purchased in the clinic to spray into the car and cage on route to the clinic, or it can be used in a diffuser in a room the day before a visit.
Anxiety medication. Gabapentin capsules can be prescribed by a vet to be given the night before and the morning of an appointment to reduce anxiety.
If all else fails, we can sedate your pet on arrival to examine them for any painful procedure (nails, sore ears etc) or blood taking. If you think they may need to be sedated, do not feed them that morning as they will be required to have been fasted to safely sedate them.
Pets
Exciting Changes at Our Cambridge Clinic: A New Lunchroom and Revamped Cattery Suites!
February has arrived, and we couldn’t be more excited to share some great news – we’re in the process of creating a dedicated lunchroom for our team! This new addition has been long-awaited and will make a positive impact on our daily operations. To make room for the lunchroom, 10 of our single cattery suites have been removed, and this change will greatly improve both the work environment for our staff and the experience for our feline boarders.
With the new lunchroom, our hardworking team members will be able to enjoy uninterrupted breaks in a peaceful space. This will help them recharge during their busy shifts, without being disturbed by the usual hustle and bustle. We know how important it is for our staff to have that moment of quiet, and this change will allow us to create a more balanced environment. Plus, our lunching staff members won’t interrupt the veterinary team while they’re hard at work – it’s a win-win all around!
But that’s not all! We’re also thrilled to announce that we’ll be putting the remaining cattery suites through a transformation of their own. With a bit less floor space, we’re dedicated to ensuring that our boarding cats have an even better experience while staying with us. Our goal is to create an enriched environment that mimics the natural behaviors of cats, so they can feel at home and more engaged during their stay.
Some of the exciting upgrades to the cattery suites include:
Wall Scratching Plates: Cats love to scratch, and we want to provide them with plenty of options to express this natural behavior.
Additional Shelving: Cats are natural climbers, and by adding more shelves, we’ll give them even more places to perch, observe, and relax in comfort.
Connecting Cat Doors: For multi-cat bookings, we hope to have the ability to connect two single suites with a cat door, giving them a larger space to enjoy together.
We understand that every cat is unique, and we’re passionate about making sure they have the best possible experience with us. By creating a stimulating environment where they can engage in natural behaviors, our goal is for every feline guest to feel relaxed, happy, and entertained.
At our clinic, it’s always our priority to not only provide excellent care for our boarders but to also create a space where they can thrive. These changes reflect our ongoing commitment to ensuring your cats are as comfortable and content as possible.
We can’t wait to share the finished results with you, and as always, we look forward to welcoming your furry friends for their next stay with us!
Pets

A 12 year old greyhound recently presented to the Cambridge clinic in distress, after falling at home & crying in pain. The dog was incredibly agitated & panting. It was noticed that the patella (knee cap) had an unusual amount of movement & there was crepitus (crunching) when the stifle and hock were flexed. The thigh was swollen, so x-rays were taken and diagnosed a pathological fracture of the femur due to weakening of the bone from an osteosarcoma.
Osteosarcomas are an aggressive form of bone cancer that primarily affect large or giant breed dogs, such as greyhounds, rottweilers, and Saint Bernards. Osteosarcomas may be found in any bones, but typically develop in the long bones, such as the limbs (usually “away from the elbow and towards the knee”). Signs of osteosarcoma include pain, swelling, or limping in the affected limb. The condition is most common in middle-aged to older dogs, though it can occur in younger dogs as well.
The exact cause of osteosarcomas in dogs remains unclear, but genetic predisposition, rapid bone growth, and trauma are considered potential contributing factors. The cancer typically spreads (metastasises) to other parts of the body, particularly the lungs, making early detection crucial for improving prognosis.
Diagnosis can involve a combination of physical examination, x-ray, and biopsy to confirm the presence of cancerous cells.
On x-ray, a bone with an osteosarcoma will appear “moth-eaten”. This is due to a process called osteolysis, which is resorption of bone matrix, and is essentially the reverse process of bone growth and development.
This leaves the affected area of the bone weakened and therefore vulnerable to a “pathological fracture”. Treatment of osteosarcomas is usually limited to amputation of the affected limb, however development of new tumors in other areas of the skeletal system is unfortunately very common.
Pets

Cows:
Heifers:
Calves/R1s:
Farming

Youngstock are an investment in your future herd. It is likely that your well-grown heifer calves have now left the home farm for grazing. Whether this is with a grazier, or on your property, you need to ensure they are set up for reaching their goal of joining the herd at the required mature liveweight.
The first challenge after leaving the home farm is continuing to grow well through summer. Calves need a consistent supply of energy, protein and fibre in the right balance to grow optimally.
There are two main reasons that calves don’t grow adequately on pasture in summer. Either they are not receiving enough pasture, or the pasture available is not suitable quality for growth.
Offering quality pasture is particularly challenging over summer when both the protein and energy content of pasture declines. To receive enough protein and energy to grow, calves grazing dry stalky summer pasture would need to eat more than is physically possible. Protein is particularly important for youngstock to develop their skeletal frame size. Failure to provide enough protein to growing calves pre-puberty can stunt growth, and this is something that cannot be corrected by improved feeding post-puberty.
Why does this matter? To achieve good reproduction in heifers, the target is to reach 60 percent of mature liveweight by mating time. A 500kg cow would need to average 700 grams per day from birth to achieve her mature weight.
Knowing the likely challenges heading into summer, declining growth rates and pasture low in energy and protein, what can we do to minimise the impacts?
As pasture quality decreases during the summer, closely monitor the pasture available. Consider other options like grass silage and well-balanced calf meals as supplements. High temperatures can reduce feed intake, so ensure calves have access to shade and cool clean water to help them cope with the heat. Weighing calves every 4 to 6 weeks to ensure they are meeting their target liveweights and identify drops in weight gains allows for early intervention. Prevent health challenges with strategies against parasites, facial eczema and trace element deficiencies.
Lifestyle
Farming

Don’t get burnt this summer!
With spore counts rising and the risk of facial eczema growing it’s important to consider purchasing your Faceguard now!
Faceguard is an elemental zinc bolus that provides up to 6 weeks protection from facial eczema in a single treatment. A further half dose delivered after 6 weeks will give you an additional 4-week cover. 10 weeks total coverage!!
There is a complete range that includes flexible treatment options for cattle ranging from 90-250kg and 251-660kg. This means the range allows treatment of calves of 90kg right up to adult cattle and bulls of 660kg.
Flexibility- Individual animal dosing is much more reliable than any trough/pasture treatment. Easy convenient dosing for all Cattle sizes from 90 – 660kgs
Longevity – A single application lasts up to 6 weeks with the option of topping up to give additional cover in a longer season.
Durability – Try as you must, but the boluses will not break when dropped!
REMEMBER - If you are bolusing on a hot sunny day leave the boluses in their polystyrene packaging with lids on as direct sunlight can soften them.
Please be careful whenever bolusing animals, whether it is zinc, trace mins, magnesium or Rumensin – we see throat injuries every year which could be avoided. Remember, don’t force it! Take your time and take breaks, it is not a fun job we know.
If you would like a hand treating your animals consider booking one of our technicians, we are more than happy to help!
Lifestyle
Farming

Sometimes you have to leave to realise that there is no place like home!
Having just returned from a two year working holiday in England, I don’t have many NZ relevant case studies for this time of year. I do have a plethora of photos of the variety of animals I saw while working in North Yorkshire. I apologise if you were hoping for an in-depth article on cancer eyes.
Sheep were a major portion of my work, the variety of breeds within the small area where I worked was impressive. From the dale-bred Mules, local Teeswaters, and rare breed Ryedales; it seemed like every second farmer had a unique breed of sheep!
Dairy practice is quite different as most of the dairy herds are housed and on a total mixed ration. Many of the farms had milking robots to reduce staff requirements. Some farms even had robots for pushing up feed and cleaning yards. Year-round calving meant you could calve a cow and then turn around and be presented with a late lactation sick cow at the same visit. Vaccination recommendations and animal health protocols made up a large portion of the vets work, especially for the high input/high output herds.
A large proportion of beef herds (suckler cows in English lingo) meant lots of caesarians in spring! There were some calls I turned up to where the cow was clipped and prepped for surgery before I even got there. The largest was a 74kg calf that had to be delivered with the help of 2-3 other people to lift the calf out of the side of the heifer.
While in the UK, I trained and was certified to TB test cattle and buffalo. Buffalo are very similar to cattle in terms of husbandry and disease, they are just more stubborn and tend to sit down when they don’t want to move. You can imagine how annoying that is when trying to move them through a crush.
Living overseas and working with a new system of farming was an excellent learning experience. UK farmers and vets are very good at monitoring disease status and using vaccination to reduce the number of cases and severity of disease. Some of this is not directly applicable to NZ, but it has helped me to think more critically about how and why we do what we do.
As well as deepening and widening my understanding, it has also increased my appreciation for NZ! There are many benefits to being an island, biosecurity being one of the biggest. Diseases like Louping ill, Anthrax, Bluetongue and Brucella are rare or exotic and mostly we don’t have to worry about them.
Farming

COWS
Plan for pregnancy testing – Six weeks after the last mating is the earliest that empties can be called. Please book your scan in early so we can give you the date and time of your choice. Most farms will need 2 scans for accurate ageing of all cows (the window is 40 to 90 days pregnant). After 100 days pregnant the accuracy of aging decreases. Make sure ear tags are clear & readable, replace any missing tags, and sort out any MINDA queries, double-up cow numbers, etc, to make the scanning day smoother and to make sure the information flows correctly when synchronising into Infovet.
The facial eczema season is coming – the best way to know if you need to start zinc is to bring in some grass so we can perform a spore count for your own farm. A week after you start providing the cows with the full recommended dose of zinc, you should check to see if the cows are actually getting this zinc at a therapeutic level, by either blood testing 10-15 cows, or doing a bulk milk zinc test. The cows must get zinc at the correct level, or they will not be protected against facial eczema (and you are wasting your money).
BMSCC is starting to increase for some – we have several trained mastitis assessors within the clinics to help keep a lid on it. Some milk cultures are a good place to start, along with a Mastitis Warrant of Fitness.
Plan your autumn-calving drying off – work out timings to allow for any dry cow withholdings and remember to order product early.
HEIFERS
Pregnancy testing heifers is important. Heifers, too, can be pregnancy tested from as early as six weeks after removing the bull. Keep a watch for any early abortions – diagnosis of a cause usually requires both blood from the heifer and fresh aborted material.
Have a summer feed plan with your grazier in case feed gets short – everyone likes to know so they can help early on rather than seeing under-sized animals returning home.
CALVES
Get them ready for grazing, and let the grazier know their status: lepto / 5 in 1 / BVD vax / last drench / last mineral treatments (copper capsule, B12/Selenium injection) so they can carry on after your hard work rearing them through spring. We have Animal Health Arrival/Departure cards which can capture this information for the grazier.
Weight gain and growth is key. Regular weighing will help identify those that are struggling and will allow targeted feeding or other interventions to make sure none are falling behind.
Lepto vaccinations are continuing: 4 – 6 weeks in between first and second ( + BVD + Salmonella…).
There's been a couple of pink eye cases in calves, outbreaks can occur if it's not dealt with promptly. The pinkeye vaccine is not available at the moment, so early detection and treatment is key.
Look after yourselves in the sun (when it’s out!), and hopefully you each enjoy a break off farm at some point.
Have a wonderful Christmas and New Year!
Farming

Lameness in our dairy herds is a persistent and consistent problem for most. Lameness can be reduced with excellent stockmanship, but is it fair enough to say we will never be without lame cows?? I think so.
So, if lameness is going to be a persistent problem, then the way we treat lame cows is very important. It’s imperative to identify lame cows early, effectively treat them, and minimise their time out of the main milking herd.
Also, is it safe to say that no one “loves” doing lame cows?? I don’t mind it, I find it satisfying to relieve the pain from the cow, but I’m not going to say that I love it. This emphasises the importance of having a simple and efficient process for treating lame cows. This is my process:

And…. That’s about it for most cases.
Some helpful tips:
Please give us a call at the clinic if you want us to give a demonstration to your staff on some of your lame cows.
Farming

‘A cow with long hooves or lameness drains every farmer’s finances. I frequently share this advice with my clients: neglecting hoof care leads to adverse financial results. No calculator can show positive numbers when it comes to lame cows.’ (Koos Vis, Diamond Hoof Care)
As an industry, our ultimate responsibility to dairy animals is their welfare, and this is non-negotiable. It is a bonus that we also make better profits.
Our challenge is to resist willful blindness – if you cannot decide if a cow is lame or not, then she is lame. When it is obvious and she is limping, we are days late in detection.
The hoof wall grows about 5cm per year. The inner and outer claws generally wear away at a different rate which leads to some areas being higher as the hoof changes shape. This changes hoof angle and weightbearing, leading to strain and damage to both hoof and limb. Comparable to us wearing odd shoes and walking on our heels.
There are three bones in each claw in the hoof, equivalent to our toe.
‘Teetering on their tiptoes like a 600kg ballerina is no mean feat for our wonderful cows.’ Tomas James, LLM UK
The discomfort of long claws reduces feed intake even in the face of adequate rations. When feed is tight, she cannot harvest sufficient nutrients to maintain either milk production or body condition. Down goes your profit, up goes your workload, down goes your morale, up goes your costs.
If we continue to turn a blind eye, the compromised hoof is likely to break apart with white line disease and sole ulcers. More misery for cow and staff, more work and cost for less return; dramatic plunge in profit.
I recently visited a mixed age cow whose gait was getting so slow she could barely get to the shed before milking was over. The photos below demonstrate just how overgrown her toe had become.


Because we didn’t have access to a handling crush with supportive limb and belly belts, the first trimming aimed to debulk the claws. This kept the time on three legs to a minimum so that she could cope with the discomfort to her hoof, hock, stifle and hip joints. Furthermore, tying the leg to rails invariably impedes access with both knife and grinder, making the work slow and laborious. Hoof trimming is an art best done with good light and 100% access to all parts of the claw, for both trimming decisions and assessment.
Once she settles into her ‘temporary feet’ we will return to further shape and optimise weightbearing of the wall, until she can grow out new hooves and restore limb posture.
Farming

COWS:
YEARLINGS:
CALVES:
https://www.vetora.co.nz/news-and-resources/grazing-departure-form
https://www.vetora.co.nz/news-and-resources/grazing-arrival-form
All the best for the rest of mating.
Farming

In late November last year, on an otherwise quiet weekend on duty I received a rather alarming call out during the middle of afternoon milking for multiple cows down on the yard and race. Any herd level event with collapsed cows is considered a high priority emergency, and is often associated with feed or toxicity.
Upon arrival I found the shed was going, and cows were walking out the exit race without much fuss, but they appeared twitchy and stiff legged. Cows rowed up for milking appeared fine from a distance, but on closer inspection had a subtle head bob that worsened when they turned their heads towatch me. The herd had been absolutely fine in the morning, but in trying to get them to the shed this afternoon some would intermittently fall over on the race and be unable to rise. The same happened on the yard when the backing gate was put on, or when cows pushed to exit the shed. If left alone for long enough the down cows would eventually rise under their own steam and carry on like nothing had happened.
All of this together indicates a simple, but frustrating disease we more commonly see in calves – Ryegrass staggers. Not to be confused with grass staggers (which is caused by low magnesium) ryegrass staggers is caused by a toxin called Lolitrem B, and is characterised by an intention induced tremor. This means that the faster an animal tries to move, the worse the tremors become, but an animal standing still in a paddock will have next to no clinical signs of the disease.
Lolitrem B is produced by a fungal endophyte in many ryegrass pastures. The endophyte is included to reduce insect damage to growing pasture, and the toxin it produces is most highly concentrated in the base of the leaf sheath and in the flower heads. The toxin has no long lasting effecton the nervous system, and once removed from the unsafe pasture cows will return to normal fairly quickly. Most of the damage to stock with this disease process comes from misadventure – animals fall into drains or fences and are unable to get out.
Unfortunately, there is also no easy fix for ryegrass staggers except for removing the source of exposure, which is difficult in a pasture-based system! Affected animals should be moved to new pasture and should not be allowed to graze close to the base of the sward. Increasing the supplement on offer will reduce the amount of pasture eaten.
In any affected mob, move animals slowly and gently, and plan for longer milking and walking times. Frustration is never a good mix with moving stock, but with ryegrass staggers in particular it will only make the ob harder. If cows go down, especially on concrete, the best option is to move away, leave them undisturbed, and allow them to rise in their own time.
Farming

Broadly speaking, mastitis in New Zealand is separated into two groups: environmental and contagious. While the majority of cases throughout the season are from environmental sources, contagious mastitis bugs are also present and can become a major issue if not identified early on. Contagious mastitis is spread from cow to cow, often during the milking process where bacteria can sit on milker’s hands or inside the liners. The major contagious pathogen in New Zealand dairy herds is Staphylococcus aureus.
Clinical signs and disease process:
Clinically, Staph aureus mastitis occurs in many forms, ranging from the suddenly collapsed cow with black mastitis, to a chronic, low grade subclinical infection. Chronic infections are the most important cause for financial losses via reduced milk production, high somatic cell count (SCC), treatment costs, and/or culling. Chronically infected cows also pose a major risk to other cows in the herd.
New infections with Staph aureus occur when uninfected quarters are exposed to infected milk. The bacteria multiply in milk ducts, leading to inflammation, blockage, and atrophy of the milk producing tissue. They can form fibrotic tissue and tiny abscesses, which are difficult to penetrate with antibiotic treatment. For this reason, Staph aureus infections tend to have a poor cure rate, and early identification and treatment is important.
Detection:
Culture has been the standard way to diagnose Staph aureus infection, however, an infected cow will only shed Staph aureus intermittently, with a peak in shedding pattern every 6.5 days. Because of this, a single culture has only a 74.5% probability of detecting Staph. This number will jump to 94 and 98% when culturing 2 and 3 samples, respectively.
Staph aureus screening can also be done during your herd test, using a test called PCR (polymerase chain reaction). Basically, the test is looking for the genetic material of the pathogen but has similar limitations as milk culture due to the intermittent shedding from an infected gland. When positive, there will be no doubt about the presence of infection. However, a single negative PCR result does not rule-out presence of “non-shedding” Staph. Approximately 70% of Staph positive cows will be identified by a single herd test.
StaphGold™ is an antibody test detecting the immune response to the Staph infection. The test has a sensitivity (true positive cows) of over 90% and the specificity (true negative cows) is very high (95%). Because this test looks for antibodies to Staph, rather than the bug itself, it is not affected by intermittent shedding.
Control and prevention:
Once a cow is identified positive, it is important that she is separated and milked last to avoid transmission to her herd mates. It is also important that all operators in the shed wear gloves. If treating, the cow should not be returned to the main milking mob until it is certain she has cleared the infection. Due to its poor cure rate and the risk to other cows in the herd, culling is often the best option for chronically infected cows.
Farming

Events that involve fireworks are a spectacular sight which most of us enjoy, unfortunately for many animals it can be a very distressing and stressful time. For our companion pets, livestock, zoo animals and wildlife fireworks can be unexpected and unpredictable. The loud bangs and bright flashes of light can be very scary and frightening.
Animals may be injured if they get too close to a lit firework or if the noise spooks them, they can run away, become disoriented and are then unable to find their way home, injuring themselves or even being involved in a traffic accident.
Here are a few ways to keep your animal safe and calm during firework celebrations
Pets

Waka – A two year old Huntaway working dog presented to our Otorohanga clinic with a harsh hacking cough and was finding it hard to bark and run without getting out of breath quickly. Waka normally loves herding the sheep and zooming around the farm, as a young dog he has lots of energy so naturally his owner was concerned about him.
When listening to Waka’s breathing with a stethoscope, the lungs sounded clear, but the trachea (windpipe) sounded harsh.
We sedated Waka so we could have a good look in his mouth/throat. Straight away we could see his epiglottis (this is the part that covers the trachea when the animal swallows and when it is open this allows air to pass from the mouth into the trachea) was swollen on the left side and covering over 60 percent of his airway. The left tonsil was also inflamed. No wonder poor Waka was so out of breath!


A needle was placed into the area where a fine needle aspirate was taken. This sample was examined under the microscope, where a lot of inflammatory cells and bacteria were seen.
This gave us a likely diagnosis of an abscess, possibly caused by eating bones that injured the throat on the way down.
Waka was prescribed antibiotics and anti-inflammatories and made a full recovery. He is back out on the farm chasing sheep and cattle, barking freely!
Pets

Catch up on the latest cases and information from our Small Animal team!

Pets

As veterinary surgeons we see cats for a variety of problems. A lot of these can be related to stress. Yes, our feline friends are very complex. Some of the well-known diseases that are stress-related are: blood in the urine, spraying, excessive grooming leading to furballs, bald patches and significant skin lesions; to name a few.
The good news is that for some cats all you have to do is improve your cat’s environment to make them happy. No medication, no diet changes.
To help you improve your cat’s environment there is a journal article, authored by feline behavioural specialists, on improving your cat’s home environment to make them happy.
Pets

Mating is upon us! Overall, most people’s cows were in good condition at calving and are milking well. Which is wonderful – but the downside is that the combination of rapid weight loss and high levels of milk production means that most people will have more non-cycling cows this season than they did last year.
Treat them early!
Things to put on the calendar for October:
COWS:
Share the link below with farm staff for a refresher: https://www.dairynz.co.nz/animal/reproduction-and-mating/heat-detection/observing-cows-to-detect-heats/
HEIFERS:
CALVES:
Hope the start of mating goes well for you all.
Farming

An oral combination drench of Eprinomectin, Oxfendazole and Levamisole with Selenium and Cobalt.
This 'new to the market' product is only available through veterinary practices and will lead the way in premium quality calf drenches.

This makes Turbo Triple Minidose the ideal treatment for routine worm control until calves reach a size that makes oral drenching difficult.
Turbo Triple Minidose offers key advantages of being a highly potent endectocide combination but with an improved safety profile when compared to an Abamectin based oral drench. It can be used in calves under 120kg body weight while also having an endectocide potency advantage over Ivermectin based oral combinations.
Eprinomectin is the most potent broad spectrum active – it can kill worms at lower concentrations of active in the animal. So, with the combination of Oxfendazole and Levamisole Turbo Triple Minidose is a major leap forward in triple active oral parasite control.
Key Benefits include:
- World first Eprinomectin, Levamisole and Oxfendazole oral calf drench
- More effective at delaying parasite resistance than single or double active products
- High Safety margin – can be used on calves under 120kg
- Developed for New Zealand conditions by a New Zealand owned company
- Includes the addition of Cobalt and Selenium
- Available in 1L, 5L and 20L packs
Turbo Triple Minidose is available at all Vetora clinics.
Farming

We see intestinal disasters reasonably often – not one a week, but probably one a month. Twisted guts, displaced stomachs, intestine that telescopes in on itself like an inside-out sock… The most common presentation seen by the vet is a cow with her eyes sunken back in her head, low temperature, rapid heart rate and a big round stomach even though she hasn’t eaten anything for 24 hours. In those cases, the poor animal is dying of septic shock and the best and kindest thing to do is put her out of her misery.
But just occasionally, we see an abdominal disaster that we can fix.
Last week I was called to see a Jersey heifer who had come in for morning milking kicking at her stomach. She hadn’t been sick for long – her udder was full of milk and her colour was good. She had a rapid heart rate because she was in pain, and when I did a rectal exam I could feel loops of distended intestine. Diagnosis: either a very recent twisted intestine or a nasty painful gas bubble. I gave her a shot of Metacam and an injection to make the gut relax, and asked the farmer to ring me in an hour with a progress report.
.png)
The Allflex collar report for this heifer. The computer diagnosed her sudden drop in eating and rumination as a heat – actually, it was due to a knot in her intestines
One hour later, the report was that she looked more comfortable but not completely happy. We decided to give her another hour.
At the two hour mark, she was about the same. Not really any worse, but not great. I went back out to have another look.
Loops of intestine still palpable on rectal exam. Heart rate high – not as high as it was before she had metacam, but nowhere near normal. She wasn’t particularly bloated – just a little bit rounder in the stomach than you would expect for a cow who hasn’t been fed that morning.
The problem with gut surgery cases is that quite often, it’s not entirely clear that you need to open them up until it becomes clear that it’s too late. Early in the course of the disease, there’s always the risk that you’ll operate on a cow who just needs to fart.
Anyway, we decided that the risk of doing nothing and having her deteriorate was worse than the risk of opening the abdomen for no reason. And having opened the abdomen, we found a couple of metres of angry looking, swollen, purple intestine, the hallmark of an intestine that has got twisted around and had its blood supply cut off. We untwisted it, pushed it back in and stitched her up. She made a rapid recovery and is doing well. Hooray!
Farming

As we head into Spring and the grass starts growing rapidly again, it’s important to consider managing the risk of bloat.
Bloat occurs when gas in the rumen accumulates in a stable foam, expanding the rumen and compressing vital organs. It is mainly caused by dietary factors. Rapidly fermentable feeds such as lush, high-protein, low fibre pastures (or legumes like clover) increase gas production in the rumen. Sudden dietary changes or overfeeding can disrupt the rumen’s microbial balance, also leading to excessive gas production.
Early detection is crucial for effective treatment - bloat can be life threatening if not treated quickly. The most obvious symptom is distension of the abdomen, especially on the left side, but early warning signs can also include rapid or laboured breathing, restlessness, reduced appetite, or excessive salivation. Severe cases can lead to sudden death due to pressure on the diaphragm and heart.
Prevention is key. Dietary/pasture management is an important tool to reduce risk – always ensure a balanced diet with adequate fibre, and gradually introduce cows to high-risk feeds to allow their digestive systems to adapt. Rotational grazing can be used effectively to limit cows’ intake of high-risk feeds. Avoid grazing on excessively lush or wet pastures if possible.
Even with ideal pasture management, often extra preventative measures are needed over high-risk periods. There are many anti-bloat products available such as Rumenox or bloat oils, which can be added to a water supply. These contain anti-foaming agents to stop the gas in the rumen forming a stable foam and getting trapped.
If an animal does develop bloat, it’s crucial to intervene immediately. In mild/early cases, an oral dose of bloat oil maybe enough to resolve the issue. In more advanced cases where the cow is severely bloated and/or in extreme discomfort, more aggressive measures may be needed. An emergency rumenotomy (stab hole into the rumen) can be used to immediately release pressure. Ideally a vet should perform this using local anaesthetic and a device that keeps the rumen open and attached to the body wall (trocar). In emergency cases where this isn’t possible, a stab hole can be made with a knife directly through the side of the cow and into the rumen. Always contact your vet if this has been done, as the wound will require stitching.
Understanding and managing bloat is essential for maintaining dairy cow health and farm productivity. By implementing effective dietary and pasture management strategies, monitoring for early signs, and having a clear treatment plan, farmers can significantly reduce the risk of bloat. Feel free to reach out to your local clinic if you would like to discuss bloat prevention or treatment options.
Farming

Watch this space!
Do you have a diabetic cat?
Are you managing them with insulin injections?
Well, in the near future, things may be changing. There is a new treatment, Senvelgo, that has been licensed overseas to treat diabetic cats. The big difference with the traditional treatment for diabetes in cats, is that you are giving the medication orally, once a day; either directly in the cat’s mouth or on their food. This will make managing these diabetic cats a lot easier for all concerned. A recent paper in the Journal of Veterinary Internal Medicine compared Senvelgo to conventional insulin injections and it was found to be non-inferior.
Read more on the study here: Efficacy and safety of once daily oral administration of sodium‐glucose cotransporter‐2 inhibitor velagliflozin compared with twice daily insulin injection in diabetic cats - Niessen - 2024 - Journal of Veterinary Internal Medicine - Wiley Online Library
Pets

It’s a busy time of year and you might not have the band width to be reading vet newsletters – but this month’s one is probably the most important of the whole year, so grit your teeth and read on!
COWS
CALVES
YOUNGSTOCK
Have a good run-up to mating!
Farming

Vetora Waikato in conjunction with Agvance have produced a range of Dairy Cow Trace Element Blends available in each clinic.
These minerals are totally soluble and can either be drenched or dosed through the water system or directly into cattle feed.
If this product is to be drenched with Magnesium Oxide it is advisable to let the Magnesium Oxide solution settle overnight before adding the Vetora mineral blend.
Magnesium Sulphate, Magnesium Chloride, salt, or Calcium Chloride can be mixed immediately.
We also have two Maize silage balancing blends available:
Maize Balancer
Containing Lime-Salt-Monocalcium, Phosphate-Magnesium Oxide
Maize Balancer DCM Plus Trace Minerals
Containing Lime-Salt-Monocalcium, Phosphate-Magnesium, Oxide, Copper, Zinc, Cobolt, Iodine, Selenium, Boron, Chromium
The Mineral blends are:
Vetora Platinum Mineral blend
Selenium, Copper (Glycinate), Iodine, Cobalt and Zinc (Glycinate)
Vetora Gold Mineral Blend
Selenium, Copper (Glycinate), Iodine and Cobalt
Vetora Gold - No Copper mineral blend
Magnesium, Zinc, Cobalt, Iodine, Selenium, Boron, Sulfur
Vetora Mineral Blend
Selenium, Copper Sulphate, Iodine and Cobalt
They all come in 25 kg bags and are administered at 5gms/cow/day. There is also a customiser service available through the clinic where mineral
levels can be custom blended to your individual herd requirements, please ask your vet about this option.
Farming

With most of your herd calved now and September arriving, your attention will be shifting to peak lactation and mating getting started. Planning is always one of the keys to success. There are a lot of ‘moving parts’ so reviewing your plan and coordinating that with your team will set your herd up for success. Complete the following animal health stock-take:

Farming

Recently, I saw a two-year-old autumn calver that had been lame for a while. The onset of lameness coincided with her spending more time on concrete. She had been transitioned onto a feed pad two weeks before calving. She gave birth to a dead calf. Due to her lameness, she was kept with a sickies mob and allowed ad lib maize. The lameness increased in severity, and laminitis was suspected. She had a corrective trim to remove overgrown horn and was turned out into a flat paddock to recover.
Despite this, the cow’s lameness worsened, especially after being walked around a concrete yard to assess her gait. She carried a lot of weight on her heels, causing the toes to be tilted upward, see Figure 1. She had an arched back when walking and was struggling to move. The prognosis was poor, and she was euthanised.

A postmortem exam showed signs of chronic laminitis, see Figure 2 and 3.


All four feet had a pink discolouration around the white line, due to haemorrhage of the corium. The corium is like the quick in the human fingernail. It supports the claw bone, contains blood vessels and nerves and is responsible for producing new hoof. Growth rings were also seen. These are grooves which occur when horn growth is disrupted. Horn typically grows ~1cm per month. So, the main laminitic event here looks to have happened ~5 months ago. Multiple rings would indicate multiple bouts of laminitis.
Laminitis is a multifactorial disease involving inflammation of the corium. Damage to the corium impairs hoof development. Where all feet are affected, it’s likely the animal has been systemically unwell. There are several risk factors for laminitis including nutritional factors (e.g. excessive carbohydrate intake/low fibre diet), metabolic disease and infections (e.g. mastitis, metritis, liver abscesses). Heifers are more prone to laminitis during calving, likely due to the massive metabolic and nutrition changes occurring. Signs of laminitis range from nothing to an animal with a stiff gait, a reluctance to move and a posture where the limbs are placed further forward than normal. It can be a single event which carries a reasonable prognosis. Alternatively, it can be a chronic illness. Once the hooves start to become misshapen, regular corrective trimming is required and they are at risk of other types of lameness e.g. white line disease and sole ulcers. This combined with the associated pain carries a poor prognosis.
Farming

We know that the calving pattern has a huge impact on herd production and sustainability.
Effective management of non-cycling cows is a key lever in maintaining (or improving) your calving pattern. The goal is to unlock the greatest cost benefit from any intervention.
A non-cycling cow is a cow that has not had an observed heat and is more than 6 weeks post calving; some of these cows will be cycling with no visible heat and some will have ovaries that have not started cycling
Checking and marking your cows on heat at least 5 weeks prior to the planned start of mating (PSM) will give you information about how ready your herd is for mating. This can be done by tail painting or using wearables data. Even if you don’t plan on doing a non-cycler treatment programme, knowing which cows have heats will give you information on what to expect for mating.
Ten days prior to mating you will have an idea about how many early calving cows are cycling. These are the most valuable cows in your herd. Ensuring that they are mated early will provide you with the best return.
The industry target is to have 75% of cows cycling 10 days before PSM. If you have less than 65% of the herd cycling 10 days prior to PSM you will struggle to get a good 3-week submission rate and have a poorer 6 week in-calf rate.
Switching your non-cycling cows to once a day at this stage has not been shown to help in getting them cycling in time. If the cows are moved to once a day, it is not recommended to move them back to twice a day for the rest of the season (I have seen disastrous results when this was done during mating).
There are a few different non-cycling cow treatment options which you can discuss with your vet. Most non-cycler programmes will take 10 days. New trial work has shown an extra 5.6% improvement in conception rates from a 13-day programme with an extra prostaglandin shot given 3 days before the CIDR is inserted.
After pregnancy testing this year, I collected the data from some of our farms which used CIDR programmes pre-mating and had an early/accurate aging pregnancy test. From this data I had 769 cows that were treated prior to PSM, with a 10-day CIDR programme that included Novormon eCG with the prostaglandin injection at day 7.
The average conception rate for these non-cycling cows was 51%. The average conception rate for Vetora farms in the first 3 weeks was 58% last season. This was a great result considering we expect non cycling cows to have lower conception rates than normal cycling cows.
Contact your vet for a reproduction consult and get ready for mating this season!
Farming

Spring always brings surprises! Early in calving I received a call out to an adult dairy cow with some unusual clinical signs. The day before her owners had noted a bit of a head tilt, and that she seemed to be consistently circling to the left, combined with her lack of appetite and the fact that she had recently calved, she had initially been treated as a metabolic cow. When this treatment did not resolve the circling, we were promptly called in for a look. In addition to the circling and head tilt, we also noted that she had mild facial paralysis on the left side, with a droopy eye and lip.
Neurological diseases are many and varied and can cause a wide range of clinical signs depending on the area of the brain which is affected, however the combination of circling, inappetence, and one sided facial paralysis is fairly characteristic for one disease in particular – Listeriosis.
Listeria monocytogenes is a hardy bacteria which is widespread in the environment, found in both soil and faeces. Soil contamination of feed is often the source of infection, cases are often associated with the feeding of poorly fermented grass silage. The low pH of well fermented grass silage inhibits the growth of Listeria, however even good silage can have areas of break down (often indicated by mouldy spots!) and Listeria can easily multiply in these patches.
Infection occurs via small wounds in the mucous membranes of the mouth or nose. Once in the body, the bacteria invade the nerve roots of one of the major nerves originating from the brain, called the trigeminal nerve and uses it as a highway up to the brain itself. This causes a meningitis, and the associated clinical signs.
Classic signs of listeriosis include:
The incubation period for infection is usually 2 weeks or longer before clinical signs start to show. Listeria infection can also cause abortions, and a condition known as “silage eye”.
Treatment involves good supportive care, anti-inflammatory pain relief, and a long course of high dose penicillin. Prognosis varies depending on how long the cow has shown clinical signs, and the areas of the brain which are affected.
Farming

When we talk about pets having worms, we are talking about internal parasites that live, for at least part of their lives, inside our pets in intestines.
These parasites can cause illness commonly vomiting, diarrhea, dull coat, anemia, and weight loss. Puppies and kittens are more susceptible than adult cats and dogs and can actually be born with a worm infection.
The most common types of worms in pets are roundworms, hookworms, whipworms and the tapeworm.

Round worm – can measure up to 18cm in length, which is often longer than the puppy or kitten it came from. These worms can infest a puppy/kitten while still in the mother’s uterus.

Tapeworms – did you know that fleas help transmit tapeworms? Tapeworms cannot develop without an intermediate host. This makes control of fleas more important. Infection occurs when the animal grooms itself and swallows an infected flea. Tapeworms are recognized easily; the dog/cat may pass segments of the worm that look like rice grains. This is not the whole worm; the rest of the worm is still inside the dog/cats intestines. The worm is obviously more common when fleas are common- in the warm humid months.

Hookworm – small worms 10-20cm long attach themselves to the intestines and consume the dogs/cats blood. Heavily infested pups/kittens develop blood-stained diarrhea. Adult pets may also carry the worm. Check your pets droppings for signs of blood.

Whipworm – seen in pups and adult dogs. The worms themselves measure 4-7cm. They cause gastroenteritis and diarrhoea. The stools are usually dark and foul smelling. These are rare to be found in cats and kittens.
Has my Pet got worms?
It is not always obvious. With puppies and kittens they can develop a big pot belly, if they have a huge burden, they can sometimes throw them up. Sometimes you can see them in your pets faeces or around the outside of the anus, but remember there will be others you cannot see.
Treatment
For puppies and kittens it is recommend to treat at the ages of 2, 4, 6, 8 and 12 weeks of age, then treat every 3 months. It is best to weigh your puppy or kitten each time before going to pick up a worm tablet, so the correct dose is given.
Treatment options are Milpro and Drontal tablets.
Pets

You may not recognise the signs of early Degenerative Joint Disease or Osteoarthritis in your pet or you may accept changes because slowing down is just part of ageing. Whilst old age is not a disease – osteoarthritis is!
Signs of pain and discomfort may be any of the following:
How can you help?
Have a discussion with your vet. One supplement option is BomaZeal™ Mobilize™ which is the only nutraceutical with an ACVM approved label claim to aid in the treatment of non-infectious inflammatory joint disease, arthritis and osteoarthritis (OA) in dogs. Proudly made in New Zealand.
Pets

Monty’s story is nothing short of remarkable. He was struck by a car and rushed to Waikato After Hours Vet Hospital.
Diagnosed with multiple fractures and severe chest and lung injuries, Monty needed immediate, intensive care. He was later transferred to our Vetora Hamilton clinic for continued management of his pain, where the goal was to stabilize him for eventual surgery.
Given the complexity of Monty’s injuries, specialists in Auckland were consulted. A CT scan revealed fractures in his humerus, scapula, and spinal vertebrae. Fortunately, his scapula and spine were stable, avoiding the need for surgery, but his humerus was severely damaged.


Two orthopaedic surgeons worked together to reconstruct his forelimb during a lengthy procedure. Post-surgery, Monty faced a strict six-week confinement period to allow his bones to heal properly. With this dedication from his owners, Monty underwent post-operative X-rays confirming successful bone union.
To aid his recovery, Monty and his owners enthusiastically embraced physiotherapy and hydrotherapy sessions. Months later, Monty has made a remarkable recovery, his playful spirit intact.
None of this journey would have been possible without the foresight of Monty’s owners, who wisely invested in pet insurance. This coverage alleviated the financial burden, enabling Monty to receive the extensive and specialized care crucial for his survival and rehabilitation. Monty’s story exemplifies the importance of pet insurance in ensuring pets like him can access lifesaving treatments and thrive once more.
- Faith Stevenson| BVSc
Pets

Pasture is a hunting ground for parasites, albeit on a microscopic level. Though many worms cannot be easily seen with the naked eye, their effects on stock can be, ranging from reduced growth rates to death.
Common signs of parasitism:
Internal parasites are shed in the faeces. Stock become infected when they graze the pasture. Young and immunocompromised animals are the most severely affected and shed the most parasites. As sheep and cattle get older, their immune system matures, and they are less affected by worms. Alpacas and especially goats do not develop a robust immunity to worms with age.
Effectively managing worms requires a multipronged approach. Below are some handy tips:
If you have any questions or want a sounding board, just call the clinic – we are always happy to help!
Lifestyle

One could argue lambing is the most beautiful time of the year but there is always a chance something could go wrong so it is important to make sure you have everything you need to intervene if necessary.
Having a lambing kit available is key. A few items to consider include:
First few days of life
Colostrum is essential to provide lambs with an adequate immune system. If they have been orphaned, not suckling on mum or do not look like they are receiving adequate amounts the best thing you can do is provide colostrum for them. Ideally use frozen sheep colostrum (or powder) but you can also use cow colostrum if needed.
Day 1 – give 5 warmed feeds spaced out evenly throughout the day. Lambs need a total of 10-15% BW of milk daily = 4kg lamb needs ~125ml per feed.
Day 2-4 – colostrum should be continued for the first 4-5 days before transitioning onto milk replacer. Larger well doing lambs can reduce to 3-4 feeds a day otherwise keep it at 5
Day 5 onwards – transition lambs onto cold +/-yoghurtised milk
Don’t forget as the lambs grow they will need more milk/day.
If your lamb is weak or collapsed give your vet a ring as a simple dextrose solution into the abdomen may be the thing that can save its life.
Bloat:
Abomasal bloat kills up to 30% of bottle-fed lambs before weaning but there is a simple fix to avoid it – yoghurtise their milk and feed small amounts more frequently rather than large ones. Bloat occurs when there is a proliferation of gas producing bacteria which feed off the lactose in milk.
Rearing lambs on cold yoghurtised milk will significantly reduce the risk of getting bloat as the bacteria in the yoghurt eat the lactose and can help reduce scouring as well. Give us a call if you would like the recipe for this method – its quick and easy and could make all the difference!
Rumen Development:
Lambs should have access to hard feed such as meal, nuts, hay from the first week of life to help develop their rumens. Provide ad lib and initially they will not eat a lot but slowly over time they will increase their intake which is critical for adequate rumen papillae development.
Tips and Tricks:
Lifestyle
Farming

Low magnesium grass staggers, also known as hypomagnesemia, is a common issue affecting cattle in New Zealand, especially in regions with lush pastures. This condition arises when cows experience a deficiency of magnesium in their system, leading to various neurological symptoms. Magnesium (Mg) is an essential element in the body and is required for helping maintain normal calcium levels, muscle and nerve transmission, energy/protein metabolism and much more. Cows cannot strip Mg from their bones like they can with calcium in times of deficit, they must get it through their diet on a regular basis.
For numerous reasons, July/August/September is a common time for this condition. Cold wet soils below 12˚C reduce the uptake of Mg by the plant. Short, lush rapidly growing pasture will naturally contain less Mg. In the first few days after calving cows will have a reduced intake resulting in not being able to eat enough to meet nutrient requirements which can be complicated with milk fever and sub-clinical ketosis. Lactation can play a factor as higher producing cows will be at more of a risk.
Clinical signs of low Mg grass staggers in cows can vary but often include:
When it comes to treatment, early detection is crucial. If a cow is displaying symptoms of Mg deficiency, prompt intervention is necessary to prevent further complications. Veterinary assistance should be sought to confirm the diagnosis and provide appropriate treatment. Treatment often involves administering Mg therapy and many cases require calcium as well.
Prevention plays a key role in managing this condition. One effective method is to provide magnesium supplementation through feed additives or mineral supplements. This ensures that the cows receive an adequate amount of magnesium in their diet to meet their nutritional requirements. Blood sampling cows pre-calving is a useful tool for monitoring Mg levels to ensure changes to supplementation are made early.
In addition to supplementation, consider the grazing risks – changing a cow’s diet from saved pasture to the 2nd round (fresh short regrowth, especially if quantity is limited) is often a big trigger for magnesium-based issues and supplementation over this period can be a cheap insurance. Monitoring the magnesium levels in soil and forage can also assist in identifying areas where supplementation may be necessary.
In conclusion, low magnesium grass staggers is a significant concern for cattle in New Zealand, particularly in regions with lush pastures. By implementing proper management practices such as magnesium supplementation, rotational grazing, and balanced nutrition, you can effectively prevent and manage this condition in your herd. Early detection, timely treatment, and proactive prevention strategies are essential in ensuring the health and well-being of cows affected by low magnesium grass staggers.
Farming

Only last week I was called out to see 2 cows on the same farm with very similar clinical signs.
Both cows were dried off mid-May and had been fine ever since and their Allflex collars had not flagged any health alerts. However, each cow had a large, very firm swelling of the maxilla (upper jaw) on one side of the face only. The cow in the photo(below) also had 4-5 areas where pus was exiting from the swelling and the discharge contained many small soft, gritty granules. One of the cows had some soft swelling behind her upper molars when I looked inside her mouth but otherwise all teeth were aligned well and there was no sign of drooling from either animal. The firm swelling was not painful to the touch and the cows were generally bright and alert.

These ‘sulphur granules’ seen discharging from the various sites are characteristic for Lumpy Jaw (Actinomycosis) and so at this stage that is the most likely diagnosis.
This condition is asporadic, relatively uncommon disease affecting mainly adult cattle. The bacteria, Actinomyces bovis, is a normal inhabitant of the mouth but needs some form of trauma to gain entry to the bony structures of the jaw. This can be due to eating sharp objects within feeds, drenching/bolus application or through tooth root injuries.
Once in the bone, the bacteria cause a chronic reaction to the underlying bony structures resulting in a firm enlargement on one side of the face and eventually small pockets of gritty pus appear at the skin surface. As is often the case in vet practice, cows don’t always read the textbooks and follow the normal clinical picture! Normally the firm swelling is present within the lower jaw but in both cows, they were swollen in the upper jaw.
Having 2 cows show up with the same, uncommon disease in the upper jaw at the same time had me stumped a little. However, on quizzing the farm owner more closely, it sounds like one of the animals has had a swollen face for a little while. They hadn’t been drenched or had a zinc bolus recently but had access to some PKE which had quite a lot of gravel in it.
We decided to try and treat both animals as they were still eating, and they were otherwise bright and alert. The decision whether to treat or not depends on the degree of destruction and deformity of the jaw.
So, a long course of Vibrostrep was initiated and at this stage it seems to be helping to reduce the swelling for both cows. Chances are that the swelling will not fully resolve but the prognosis is relatively good as long as the cheek teeth are in alignment.
The other recognised treatment for this condition is Sodium Iodide solution given intravenously. Whilst not strictly speaking an antibiotic it is often used in the treatment of both Lumpy Jaw and Woody Tongue.
Fingers crossed we get a good outcome with these cows.
Farming

Rumenox is a rumen modifier (an ionophore) that contains the active ingredient monensin. Rumenox provides more energy to dairy cows by increasing the level of propionate produced in the rumen. This energy response is equivalent to feeding an extra 1.0 kg of dry matter at a portion of the cost.
Ketosis Prevention
Sub clinical ketosis is an energy robbing disease that has been associated with increased endometritis and a decreased 6 week in-calf rate. The cost per cow with sub-clinical ketosis is $86. Rumenox significantly reduces the incidence of sub-clinical ketosis in dairy cows by making more energy available and reducing blood ketone levels, this effect has been shown in a number of NZ studies. A recent analysis of New Zealand data showed a reduction in sub-clinical ketosis by 29.6%.
For optimum results Rumenox should be introduced pre-calving or, if not practical, it should be administered into the stock water as soon as the dairy herd returns to the milking platform in early spring.
Milk Protein Production
The increased propionate produced in a cow’s rumen when Rumenox is introduced results in greater glucose production which leads to increased milk protein.
Pasture Bloat
Rumenox is an effective bloat control strategy. The fermentation shift achieved in the rumen leads to a reduction in methane gas production. This shift has a lasting effect of 24-48 hours. This duration of activity is particularly important when relying on water medication for bloat control e.g. dosatron. Cows don’t always drink regularly, in fact they drink very little on wet days. Years of observational evidence strongly suggests that monensin out performs bloat detergents when relying on water medication for controlling bloat. When treating with conventional bloat detergents cows are still vulnerable to a bloat challenge when drinking is restricted, this is due to their shorter duration of activity.
Farming

COWS:
Just for fun… the following is taken word for word from the 1938 NZ Veterinary Handbook

‘The main factor contributing to milk fever is an easy calving which makes very little call for expenditure of muscular or nervous energy.’
Who knew?
YEARLINGS+/- AUTUMN BORN:
NEWBORNCALVES:
Lastly, it’s a busy time for everyone without getting sick, so: wash hands and change overalls to keep you & your family safe!
Farming

Hi Everyone,
Hope you’re all enjoying some down-time with the cows dry. It’s been a lovely autumn – not too much mud yet! Long may it last.
Below is our e-Update for June (apologies for all the talk of preparing for calving – it seems to come around quicker every year).
COWS
HEIFERS
CALVES
Farming

A cow is classified as a “down cow” if they haven’t responded as expected to treatment or are down for more than two hours after treatment. Providing the correct care quickly can reduce complications such nerve or muscle damage, hip dislocations, mastitis, and pneumonia.
When you discover a down cow, it is important to assess her quickly – is she looking depressed or even non-responsive? Take this as a sign that she needs be urgently treated. If she is responsive, aware of her surroundings and bright, her treatment is still a high priority, but not as urgent as an unresponsive cow.
Assessing why she is down is the next step. Metabolic imbalance? Injury? Other illness? Knowing her diagnosis/prognosis will help with deciding the next steps - either treatment and nursing, or euthanasia.
When treating a down cow it is crucial to begin this process as soon as possible. Give her any treatments she may require and set her up to be as comfortable as she can. Move her to a nursing area with soft bedding where possible. Evaluate her surroundings and eliminate any risk factors that make her recovery harder or slower. Moving her is top priority if she is in a dangerous place such as close to a drain, electric fence or even if she is on a walkway as that may make her a risk to the rest of the herd. If she is down on gravel or concrete this can increase risk of more damage even if she’s only there for an hour or two. Good shelter for the down cow is required in extremely cold, wet or hot conditions.
While moving her is important, you also need to be careful not to cause any more damage and reduce her chances of recovery. Safe options include using a carry-all on the back of a tractor (safely secured), a sling, and a front-end loader bucket on the front of a tractor. Hip clamps may be used to move her short distances, but she MUST also be supported with a strap or belt.
Nursing areas need to have soft, clean and dry bedding to help reduce the load on their muscles. Having a non-slip surface will help her when she tries to stand. This, alongside a continuous supply of clean water and good feed is important.
Once she is in a suitable area note which leg the cow is sitting on each time she is checked. The circulation in the leg she is laying against may become compromised if she is unable to swap sides herself. To prevent this, roll her to the opposite side every 3 hours. Flexing her hind legs out at the same time can help minimize nerve damage. Regular hand stripping and encouragement to get up is also very important. Lifting devices must only be used to get the cow on to her feet – she must not be left hanging in the hip lifter or sling.
Cows with serious illness or injuries have a lower chance of recovery. If treatment is not a viable option, the down cow must be euthanized as soon as possible. Down cows must not be left to suffer. Call your vet for further advice.
Farming

Ensuring your calves get a great start requires focusing on boosting calf immunity through colostrum management by providing the right amount of high quality colostrum at the right time. This goes hand in hand with reducing the challenge of disease through good husbandry, hygiene, facilities and nutrition.
An additional barrier to calf scours can be achieved by vaccinating your cows prior to calving.
Calf scours are one of the most stressful and costly diseases for vets and farmers to deal with. And we know that calves that recover, grow slower and have poorer outcomes than healthy calves.
The primary pathogens associated with calf scours in New Zealand include rotavirus which is recognised as the most common, E.coli, cryptosporidia, coccidia, salmonella and coronavirus.
Cows vaccinated for scours produce high levels of protective antibodies for Rotavirus, E. coli and coronavirus generally from two to twelve weeks after vaccination so cows should be vaccinated about three weeks prior to planned start of calving to protect your calves.
Salmonella is known to cause devastating disease in the Waikato and has been implicated in abortions and severe scour outbreaks in cows and calves. Fortunately, we have a vaccine to reduce the impact of these outbreaks.
Speak to our team to about management and vaccination options to protect your cows and calves this spring.
Farming

This autumn I was called out to a heifer grazing property where three R1 heifers had been found dead within the last 48 hours.
They were all in the same mob of approximately 70 dairy heifers. The third one had been found that morning and the owners were keen to get a post mortem examination done. The animal was a well grown cross bred heifer. It was slightly bloated, with no sign of struggling or evidence of scouring. The heifers were on pasture only - quite lush because of the favourable autumn conditions.
The causes of sudden death in this age group on a purely pasture diet are quite limited. We discussed possible poisons e.g. Lead, Cyanide, Nitrate, plant poisons such as Yew, Ragwort and Oleander but the conditions were not right for any of these causes. By eliminating these the most likely cause of death in these heifers was a Clostridial infection.
Their vaccination history was uncertain. They had been vaccinated with 5 in 1 as calves but may not have received a booster vaccination. I examined the carcase for signs of Blackleg. There were no characteristic swollen muscles with gas but there was some blood-stained froth from the nose. On opening the carcase, the intestines appeared v inflamed and contained bloody diarrhoea. The kidneys and liver were also swollen and inflamed.

Most of the changes were confined to the digestive tract. The carcass was putrefying quickly considering the heifer was only found dead that morning. Samples were taken for laboratory testing to try and identify the cause. We then looked at the rest of the heifer mob and they were well grown with no sick looking animals.
It was decided to give them a booster 5 in 1 vaccination due to the uncertainty of their vaccination status. Unfortunately we did not get a definitive diagnosis from the laboratory although we were able to rule out acute Salmonellosis. From the history and post mortem signs we made a provisional diagnosis of Clostridial Enterotoxaemia , which is as nasty as it sounds!
Fortunately, the 5 in 1 vaccine routinely used protects against the strains of Clostridia that cause this disease.
No more deaths have occurred in the mob which is a great relief. This case highlights the importance of fully vaccinating calves and on affected farms considering annual clostridial vaccination of heifers and the herd.
Farming

As our pets age, we want them to enjoy their golden years, and remain as healthy and happy as possible. Although they may not need as much exercise and might be happy to sleep half the day away, we need to keep a close eye on any changes that are occurring in their bodies.
Below are some common conditions that older dogs can suffer from and signs for you to monitor at home.
Arthritis:
•Stiff, stilted gait
•Struggling to rise or lie down
•Weakness in hindlimbs
•Lameness or pain
•Reluctance to walk or play
•Unable to settle and get comfortable while sleeping
Dental disease
•Bad breath
•Tooth discolouration, tartar forming on teeth
•Red, inflamed gums
•Missing or loose teeth
•Loss of appetite
•Sore mouth/oral pain
Cancer
•Sadly there are many types of cancer that pets can get, and they all cause slightly different clinical signs and symptoms
•Any lumps or bumps should be regularly checked, especially if they are growing fast or annoying your pet
•Any weight loss or appetite changes
•Changes to your pets behaviour
Kidney disease, diabetes or other chronic changes
•These are often associated with increased drinking or change of appetite as well as weight loss.
A lot of older pets diseases are progressive and early detection allows for better quality of life and treatment options. Regular vet checkups are the best way to ensure your pet is as healthy as they can be, and to discuss how to ensure your pet is happy in their golden years. Blood tests or other diagnostic tests may be recommended to help the vet diagnose any conditions early on, and blood tests can be run during a consultation.
Vetora are running a Golden Paws promotion in May to help us look after your older pets - both dogs and cats. Please call your clinic to book in for this promotion.
Pets

Hi Everyone,
What a lovely autumn we’re having – it’s such a pleasure after lots of droughts in recent years.
We’re seeing a few cases of facial eczema around the place, unfortunately it takes more than a few chilly nights to destroy all those spores. Some herds have blood tested all their cows as part of a particularly cool trial with LIC looking at inherited resistance to facial eczema, and we’ve been horrified at the number of perfectly healthy-looking cows with blood results showing they’ve been badly hit. No wonder that often cows don’t milk, and young animals don’t grow as well as we think they should at this time of year, even when they’re being really well fed.
Below is our mid-month dairy vet e-Update for May:
COWS
HEIFERS
CALVES
All the best for the rest of May.
Farming

With Spring calving approaching fast and most cows now dry, it is a good time to check your herd vaccination status and catch up on these if needed.
There are many vaccinations available, so it is worthwhile talking to your vet about what is best for your herd and farm, depending on your individual risks.
Briefly, the options and rationales are as follows:
Leptospirosis vaccination
Leptospirosis infection, potentially caught from infected cow urine, is a major human health and safety issue, which in some individuals can cause severe flu-like symptoms, and even death. The vaccine does confer some protection to the cows to help prevent various symptoms of infection, including decreased milk yield, blood in the urine, anaemia, and abortion. However, the primary reason to vaccinate your herd is to protect farm workers, and anyone else who may come into contact with your cows (or their urine).
Scour vaccinations
If you have ever dealt with a major outbreak of calf scours, or if you want to avoid such a traumatic and devastating event, then consider vaccinating your herd with a scour vaccination – these cover for Rotavirus, Coronavirus and E coli (but NOT cryptosporidium). Calves can become infected from carrier cows (no symptoms), other calves, or from an infected environment(incorrectly cleaned calf sheds). Vaccination does not eliminate the diseases on its own, but is a tool to help reduce the risk, in conjunction with strict hygiene, and meticulous colostrum management.
Salmonella vaccination
Salmonella infection can result in a sick cow, often very unwell, with a high temperature and profuse diarrhoea that may include blood, mucus and rotten intestine. Death may occur without early treatment. Salmonella can be caught from the environment, contaminated water or food, or more likely from carrier animals who shed salmonella in their faeces in times of stress.
BVD
Bovine viral diarrhoea virus (BVD) is a complex disease that can cause usually mild gastro symptoms in young stock and dry cows, but in pregnant cows it can cause reproductive losses, abortions, and the birth of unthrifty calves and persistently infected (PI) calves. Vaccination is part of your BVD control toolkit, which also includes biosecurity measures, BVD bulk tank milk monitoring, and removing PIs from your herd.
Clostridial diseases
This is a group of diseases that includes tetanus, blackleg, malignant oedema and others. Infection is from spores in the environment. Animals are usually found dead, though there may be some signs that indicate a clostridial disease was responsible, otherwise it is difficult to definitively diagnose clostridial disease. A number of “random” sudden deaths on farm may in fact be due to clostridial infection. Calves are routinely vaccinated, but it is good practice to vaccinate the herd too. The vaccine is relatively cheap, so if an average dairy farm were to lose one cow every two or three years to a clostridial disease, the vaccination would be economically worthwhile.
Other injections
While we are on the topic of turning cows into metaphorical pincushions, trace element supplementation should also be considered, and injections are available for copper, selenium and B12, or as Multimin (copper, selenium, zinc, manganese).
Lifestyle
Farming

An oral combination drench of Eprinomectin, Oxfendazole and Levamisole with Selenium and Cobalt.
This new to the market product is only available through veterinary practices and will lead the way in premium quality calf drenches.
Once calves have developed enough immunity to coccidia infection, after treatment with Turbo Initial, then with to Turbo Triple Minidose. Animals remain very susceptible to gastrointestinal parasitism but will still be young enough to treat with an oral drench.
This makes Turbo Triple Minidose the ideal treatment for routine worm control until calves reach a size that makes oral drenching difficult.
Turbo Triple Minidose offers key advantages of being a highly potent endectocide combination but with an improved safety profile when compared to an Abamectin based oral drench. It can be used in calves under 120kg body weight while also having an endectocide potency advantage over Ivermectin based oral combinations.
Eprinomectin is the most potent broad spectrum active – it can kill worms at lower concentrations of active in the animal. So, with the combination of Oxfendazole and Levamisole Turbo Triple Minidose is a major leap forward in triple active oral parasite control.
Key Benefits include:
- World first Eprinomectin, Levamisole and Oxfendazole oral calf drench
- More effective at delaying parasite resistance than single or double active products
- High Safety margin – can be used on calves under120kg
- Developed for New Zealand conditions by a New Zealand owned company
- Includes the addition of Cobalt and Selenium
- Available in 1L, 5L and 20L packs
Turbo Triple Minidose is available at all Vetora clinics.
Lifestyle
Farming

It was typical day in May, very overcast and foggy conditions and I was called to check out a sick cow. She was a Friesian Jersey cross bred cow, 5 years old and recently dried off. She had suddenly started scouring the previous day. The faeces were very loose, a light green colour with some blood present. The temperature was normal at 38.6C and the heart rate was elevated to 80 beats/min. The cow appeared to be fully hydrated despite the acute scour. All the other herd members appeared to be healthy and unaffected.
A faecal sample was taken for salmonella culture and a blood sample was collected for Johnes disease testing. The cow was also confirmed as pregnant from rectal examination.
Treatment was started with an injectable antibiotic and Ketomax an anti-inflammatory drug. Oral fluid therapy is often given to suspect salmonella cows but was not required in this case.
An unusual Salmonella species was cultured at the animal health laboratory which was then sent to the ESR Wallaceville lab for salmonella serotyping. The Johnes blood test result was negative. Ten days after the faecal sample being collected the salmonella bacteria was fully identified as Salmonella Give. This is a relatively new salmonella serotype in New Zealand cattle that has increased in the numbers of affected herds in the last few years. In other herds that have had Salmonella Give, the bacteria causes scouring cows and also abortions in some cows. Salmonella Give can also result in scouring, septicaemia and death in young calves.
The dairy farmer was reminded that Salmonella is a zoonotic disease and can affect people with acute vomiting, diarrhoea, abdominal cramps and septicaemia. In salmonella outbreaks we advise that gloves and PPE are worm by all farm staff and hands are carefully washed and cleaned prior to eating or drinking. Salmonella is also excreted by infected animals in the milk, so raw milk from the vat should not be consumed by any farm staff. Health & safety notices should also be displayed in the shed advising on the salmonella risk to people and that no eating or drinking is allowed in the shed.
Farms affected with salmonella are requested to notify their milk and meat supply companies to enable these organisations to take food safety precautions.
Advice was also given on removing any aborted material from yards and paddocks should any cows abort.
Salmonella vaccination provides good protection against the specific salmonella serotypes of Bovis-morbificans, Typhimurium, Hindmarsh & Brandenburg. There may be minor cross protection from these serotypes to Salmonella Give. The farmer decided to go ahead and vaccinate the herd for salmonella. All the cows and heifers were given two vaccinations 4 weeks apart.
The affected cow made a full recovery and no further cases of salmonella occurred in the herd which was an unusual outcome, however vet and farmer were both very grateful and relieved!
Farming

COWS
HEIFERS
CALVES
All the best for the last few weeks of the season.
Farming

How did scanning go this year?
Every scanning season we get asked how the results have been going so here is the answer. Across our clients there is a wide range in performance. Below is a graph showing the 6 week in calf rate for Vetora Waikato clients for 2023 mating. Each farm’s result (total of 244 farms) is shown as a vertical blue bar from the lowest (37%) to the highest (85%). The average across all farms was 69% (blue horizontal line). The industry target is 78% (green horizontal line).

The range in empty rates is even more variable and depends on mating length. The take home message is that for the majority of our herds there is huge potential for improving the 6 week in calf rate and empty rate.
How to improve your herd repro results
There are many ingredients that go into making a good repro cake in your herd, from BCS to genetics to how young stock are grown out. Some ingredients will be more important for your herd than others. To get an idea on where to start, work through your fertility focus report with your vet. This report gives a great overview of which ingredients are already working and which ones can be improved.
Once you have identified what you want to work on you can choose how you want to work on it. Just because you are getting advice from a vet doesn’t mean you’ll be doing more metrichecking and CIDRs. The main thing to remember is that improving repro is a long-term game and it will take more than one season to get real results.
A case study
The case farm is spring-calving and milks around 700 cows. The graph shows the in calf rate by week of mating for the last 3 mating’s compared to the industry target. The 2021 results were 69% 6 week in calf rate and 23% empty (77% in calf) after 9 weeks. Before mating 2022 the herd was fitted with collars but mating performance got worse. The collar data was used to identify the issues and a plan was made for 2023 mating specific to the case farm. The result was a 12% increase in 6 week in calf rate and 12% drop in empty rate (although mating was 1 week longer).
Using the industry figures of $4 per % improvement of 6 week in calf rate and $10 per % improvement in empty rate multiplied by herd size, the value of the improvement was worth around $115,000.
The next step for this farm is to review the 2023 collar data and make a plan to get another step closer to the herd’s potential.

Farming

As many of you might have heard already, the criteria for authorising dry cow therapy has changed. Last year the Veterinary Council updated their professional standard for veterinarians regarding authorising dry cow therapy. The Veterinary Council of New Zealand is a body which upholds and regulates veterinary standards. It is the body in which veterinarians must be registered to in order to practice in New Zealand.
The new standard released can be found at https://hub.vetcouncil.org.nz/authorisation-of-dry-cow-therapy.
A big part of these changes is to ensure antibiotic therapy is only used in infected animals. Overuse of antibiotics leads to antibiotic resistance. Blanket dry cow therapy means a lot of healthy (non-infected) animals get antibiotic treatment that they do not need thus increasing antibiotic exposure and chance for resistant bacteria.
High risk farms have a higher chance of having infected animals fall into the ‘clean cow’ category. Therefore, these farms will still be allowed to do blanket antibiotic therapy. The high-risk farms will have at least 3 of the following criteria:
· BMSCC average above 250,000
· More than 2% of herd with mastitis over the dry period
· More than 10% of herd had mastitis in first month of lactation.
· More than 25% of herd over 150,000
· More than 15% of cows had a significant increase ISCC over the dry period (going from <150,000 at last herd test to>150,000 at first herd test of season)
Farms with a blanket dry cow authorisation will need to be making steps towards resolving these mastitis issues, for example doing cultures, antibiograms, or mastitis WOFs.
Internal teat sealant when used correctly are effective in reducing cases of mastitis over the dry period and as cows are calving down. It provides a plug to stop new infections entering the udder which gives long term protection up until the point of calving.
However, there can be a great risk in using teat sealant alone if not done correctly. Administration of internal teat sealants must be done to an absolute gold standard to avoid severe mastitis. Without the additional coverage of antibiotic dry cow, careful attention to cleanliness and good technique as well as good pre and post dry off management is essential to avoid a poor outcome. The tubes need to be kept clean and dry to avoid any contamination of the tube. The teat end must be completely clean. There are bacteria all over the skin surface. When the tube enters it can push bacteria/yeast/other microbes that are on the skin up into the teat canal. So, the teat end needs to be clean and then another teat wipe used to sterilise, and then the tube can be inserted. It is important to concentrate on making sure the teat sealant tubes tip doesn’t come into contact with anything other than the clean teat end.
We can provide on farm training to all staff involved in drying off the herd. We also have technicians which are all trained and assessed at the start of each season who can do the teat sealant administration for you. Correct teat sealant administration is crucially important.
Farming

Johnes disease is a chronic infectious disease of cattle (and other ruminants) characterised by diarrhoea and wasting. It is caused by the bacteria Mycobacterium avium subspecies paratuberculosis .
Johnes is a poorly understood and often largely ignored disease due to its slow onset and long incubation period but it can be costly in terms of production losses and premature culling of animals.
There is also an increasing concern to food safety authorities and the consumer public with the similarities between Johnes disease in cattle and Crohn’s disease in humans. There is ongoing debate as to whether there is an identifiable link between these two diseases.
It is generally accepted that calves are infected before or at birth or can be infected up until about 12 months of age when they become more resistant to becoming infected. They are most likely to be infected in the first few days or weeks of life by:
1) Transplacental infection from infected mothers
2) Drinking infected colostrum or milk
3) From faecal contamination of teats, grass, or water
4) By the respiratory route.
The most important and common route of infection is 3) the faecal/oral route.
After infection there is a long incubation period and it is not until around 3 years of age or older that cows will become “clinical”; losing weight, dropping production and a profuse scour (sometimes referred to as a “pipe scour”). This scour ends up shedding large numbers of bacteria especially after a period of stress, (e.g. Calving) which then contaminates the environment.
As the disease progresses the lining of the bowel becomes thickened resulting in malabsorption of nutrients with fluid and protein loss from the bowel.
With Johnes disease; cows aren’t usually “off colour”, generally have a normal appetite, and are bright until the latter stages which can be 1 to 6 months or longer.
The number of cows showing clinical disease is generally a small percentage of the total number of animals infected with the bacteria.
There are no effective treatments for Johnes disease so once a diagnosis is made the animal should be culled to limit the contamination of the environment and spread to other animals-especially calves.
Testing of individual animals can be done by blood test or herds can be screened by an individual cow milk test with a follow up blood test for those found to be positive or suspicious on milk test.
Control of Johnes is best achieved by:
1) Early identification and elimination of infected animals
2) Reducing faecal/oral spread by having clean calving areas, not allowing or limiting time that newborn calves can suckle from their mothers, feeding colostrum from low-risk cows, ensuring feed and water is not contaminated with faeces, and limiting calves’ contact with cows’ faeces (effluent paddocks).
3) Management of milk and colostrum intended for consumption by calves either by the use of calf milk replacers or by the use of colostrum and milk from low-risk cows after thorough cleaning of the teats and udder before milking.
If you feel that Johnes Disease could be a significant problem in your herd with a number of fading and scouring cows then contact us to have a chat and make a plan.
Farming

So . . It’s that time of the year again where we start to think about heifer teatsealing.
This year we are encouraging our farmers to get in early to get the most benefit out of teatsealing their heifers. Heifers are your future herd in which you have invested a considerable amount of money prior to them entering the herd. This means we want to avoid heifers developing mastitis post calving to reduce them being culled early.
Heifer mastitis rates on some NZ farms have reached 25% so it is important to try to minimize this problem and the costs associated with it. Teatseal is a non-antibiotic that is inserted into a heifer’s teat canal to form a physical plug preventing bacteria from entering the udder leading to a 70% reduction in clinical mastitis.* Using it anytime from 1 to 135 days prior to calving*is just as effective in reducing the risk of clinical mastitis up to 30 days after calving. (*NZ published studies)
Why would you want to get it done early?
• Get the most out of the product and cost itself.
• Can be done during less stressful times of the year (pre herd dry off).
• Lower risk of clinical mastitis within the first 30 days of calving when does earlier.
• Use of the trailer is available at any time if there is a race and yard set up.
We have two purpose-built trailers up and running between the Vetora teams. The trailer allows us to teatseal 5-6 heifers at a time at nearly any location which has access to yards and a race.
Benefits of using the trailer:
• Don’t need to train through shed (time consuming)
• Used to going up races due to previous health treatments
• Can be done off farm at grazing before returning home.
• A lot safer for both the techs and heifers due to the structure of the trailer.
If you would like to get in early or have a chat with our teams, please feel free to contact us at any time.
Farming

With Autumn approaching, herd Leptosporosis vaccinations are just around the corner. Leptosporosis (lepto) infection is spread by contact with urine of an infected animal, either directly or indirectly (eg. from contaminated water). In young calves, lepto can cause fever, “red water” (discoloured urine), and loss of appetite. Less commonly, adult cattle can be affected causing reproductive losses, sudden decreases in milk production, and jaundice. Human infection with lepto can be severe, causing flu-like symptoms and in some cases hospitalisation.
Traditionally herds have been vaccinated with Lepto 3-Way, however, Lepto 4-Way has recently come onto the market. Lepto 4-Way offers protection for all three strains present in the 3-Way vaccine (Hardjo, Copenhageni and Pomona) as well as the strain Pacifica.
Lepto Pacifica has been labelled as New Zealand’s emerging lepto strain, with recent research suggesting that Pacifica could be present in almost 75% of dairy herds. Cases of lepto in dairy farm workers on vaccinated farms have spiked in the last few years, suggesting many of these infections may be from this new strain, and often with more severe symptoms seen. Cattle seem to be the “maintenance” host for this type of lepto, so do not show signs of disease.
Vaccinating cattle with Lepto 4-Way provides an immune response against the Pacifica strain, reducing shedding in the urine, helping to protect farmers, workers, and other people on farm from being infected.
Because the Pacifica strain has not been available in vaccines before and the vaccination does not contain live bacteria, a booster in 4-6 weeks after initial vaccination is required. This stimulates the body’s “memory” to provide immunity until the following annual booster. In calves, it is important that the vaccination programme is started early to limit the risk of animals becoming carriers of lepto prior to vaccination.
While vaccination for lepto is important to limit the spread of disease, other factors for protection need to be considered as well. Staff training is important to make sure everyone is aware of lepto and the risks; avoid contact with urine by wearing appropriate PPE and implement good personal hygiene. Lepto can survive in wet conditions for up to six months, so effluent and waterway systems need to be well managed. As rodents can be hosts for some strains, bait stations should be well maintained, and food sources need to be rodent proof. New stock on farm should be vaccinated prior to entry, and if there are sheep, deer or pigs on farm they should also be vaccinated.
Vetora will start using Lepto 4-Way this year, with 2024 born calves being vaccinated and boosted with the 4-Way, and herd immunity developing over successive years. If you’d like to jump straight in to vaccinating your herd with Lepto 4-Way, we can organise a booster shot for the herd four to six weeks later.
Farming

COWS
HEIFERS
CALVES
We are looking forward to catching up with everyone soon during RVM consults!
Farming

The time has come to protect your animals against facial eczema. This is a disease that can affect sheep, cattle, alpacas and deer, causing serious damage without an effective preventative plan in place. It can occur when animals ingest fungal spores which grow at the base of grass swards in warm humid conditions especially during the months of January through April. When the spores are ingested they release a toxin (spore desmin) into the bloodstream which accumulates in the liver, causing severe damage. Exposure to large number of spores can damage the liver but regular exposure to moderate numbers can do the same. It is highly recommended to bring in grass samples from where your animals are grazing so we can look at the level of spores on your property and assess your risk level.
The damage to the liver can lead to:
This is a painful condition for the animals and only 20% of them show the typical facial eczema skin lesions so it often goes undetected.
Prevention is key to successfully protecting your animals against this condition and zinc is the best way to do this. Contact your vet to discuss the best way to give zinc to your animals. It is critical to provide shade and avoid grazing paddocks too low as this is where the highest number of spores reside. Providing supplementary feed such as hay and silage over this high risk period is also a good idea to help dilute the number of spores ingested.
Lifestyle

Ryegrass staggers is a disease caused by a fungus which can grow in perennial ryegrass producing a compound toxic to the nervous system. The fungus is found in all areas of the plant but mostly concentrates in the seed head and base of the leave in the grass. Clinical signs will usually develop within 2-3 days of ingesting the pasture.
The main clinical signs seen closely resemble a “drunken” animal including:
Unfortunately, there is no specific treatment, but supportive care is required. It is important to remove the animals from the affected pasture but vital to reduce their stress while doing so to avoid collapse. Affected stock can suffer from misadventure through drowning and getting caught in hazards, so ensure they are put in a safe paddock.
Treatment:
Diagnosis is usually made through clinical signs along with diet and the recent weather conditions. It is common to find multiple animals affected if they are eating the same pasture.
Prevention requires avoiding overgrazing so the animals cannot eat to the base of the grass and cut hay or baleage before the plant can flower to help minimize the toxin in the plant. Mixing your pasture with other grass species and legumes will also help to reduce intake of the fungus.
There are plenty of toxic plants/substances that can cause these clinical signs and may require different treatments so give your vet a call if you are concerned so we can make the correct diagnosis and help your animals to recover as soon as possible.
Lifestyle

Cows:
Heifers:
Calves/R1s:
Farming

Woody Tongue is a relatively common disease in cattle. It is a bacterial infection caused by a pathogen called Actinobacillus lignieresii. This bacteria normally lives in the cow’s mouth without causing any trouble, but when there is damage to the tongue or inside of the mouth, the bacteria takes the opportunity to invade the damaged tissue and start a particularly painful infection. The damage usually comes from coarse feed, gravel or weeds. The affected tissue appears massively thickened and is very tough. It often appears yellow as it contains many small abscesses and may have associated ulcers. Externally you may see swelling and drooling, and you will likely see a drop in production as the cow won’t be eating much due to the pain. The bug that causes Woody Tongue is not susceptible to treatment with many types of antibiotics, but when the correct drugs are used this condition is usually treated successfully. It is important to include some form of pain relief in your treatment of Woody Tongue as it is exceptionally painful.
There are several viral diseases in New Zealand that can cause lesions that look similar to Woody Tongue, including BVD and MCF. It is highly important that a veterinarian rules out these conditions as they will not respond to routine treatments, and there is risk for them spreading from cow to cow. Although not present in New Zealand, Foot and Mouth disease can cause ulcers that are similar in appearance to Woody Tongue. Foot and Mouth disease poses significant economic and animal welfare risk to New Zealand’s livestock industry so it is important we investigate mouth issues thoroughly to rule out FMD as a possibility. There are also a number of other diseases that cause swelling under and around the jaw. These include Johne’s disease and heart failure and are very commonly misdiagnosed as Woody Tongue by farmers.
Lumpy Jaw is another condition that can look quite similar to Woody Tongue, however this is caused by a different pathogen which can behave differently. The way in which an infection occurs is much the same as with Woody Tongue, but this bug (Actinomyces bovis)typically won't just stop at the soft tissues in the mouth and will spread infection to the bones of the jaw and face. The infection can cause permanent changes to the shape of the bones that you may notice externally. This change is irreversible. Lumpy Jaw doesn’t respond well to antibiotics, the recommended treatment is a highly irritant injection that should be given by a vet, but even then is not guaranteed to resolve the problem completely. If treatment is started earlier in the course of disease, success is more likely. Once again, the provision of pain relief as soon as the problem is noticed is paramount due to the highly painful nature of the condition.
Ultimately, there are a number of diseases that affect the mouths of cows, most of which are very painful and can cause dramatic issues with the welfare and productivity of affected animals. Some can be very insidious and may not respond to routine treatments. A quick and accurate diagnosis can be achieved by calling your vet out as soon as symptoms are noticed and gives the greatest likelihood of providing a successful treatment and more rapid return to normal function.
Farming